Organizations that have not already transitioned to using wRVUs from the current Medicare Physician Fee Schedule (MPFS) should plan to make the switch sooner rather than later.
Due to the complexity surrounding this issue, many organizations continued to utilize the 2020 MPFS to calculate wRVUs for production-based provider compensation plans in 2021. In the short term, this ensured providers would continue to earn at historic compensation levels for similar volume. This also gave organizations time to conduct analysis and develop strategies for adjusting compensation parameters to coincide with the MPFS transition.
This was an effective approach last year and allowed many organizations to successfully transition to the new fee schedule. Based on our survey of 68 clients and colleagues, 58% of organizations implemented or planned to implement the new wRVU values by the end of 2021. (Figure 1) This leaves 42% of organizations who have pushed off implementation to 2022 or beyond.
For organizations still operating under the 2020 MPFS wRVU values, MPFS transition should be a 2022 priority. While maintaining 2020 wRVU values was a useful temporary measure, it is not a viable long-term strategy.
The changes introduced in the 2021 MPFS represent a paradigm shift; outpatient office visits generate up to 46% more wRVUs compared to the 2020 fee schedule. The magnitude of this changes requires that organizations adapt soon. By delaying the transition, organizations are effectively kicking the can down the road and making it even more difficult to implement future fee schedule changes Meanwhile, organizations that have adapted to the sweeping changes caused by the 2021 MPFS will be in a better position to successfully implement new fee schedules as CMS undoubtedly makes minor tweaks in the years to come.
Organizations seeking to transition to the new MPFS in 2022 have the advantage of benefiting from the experiences of those who have already been through the process. During the past year, the team at HSG has worked with many healthcare systems on this compensation issue. We recommend a structured, data-driven approach to determine the appropriate compensation adjustment strategies. Ultimately, hospital and health system leadership must determine the desired philosophical approach to adjusting per wRVU compensation rates as the organization transitions to the new fee schedule. HSG has identified a continuum of approaches, with three key categories:
- No adjustment - compensation rates will remain constant when implementing the new wRVU values. This means providers' compensation will increase in proportion to the increase in wRVU values.
- Budget neutral - most or all of expected revenue increases will be shared with the organization’s providers. This means providers’ compensation will increase in proportion to the increase in Medicare revenue.
- Compensation neutral - providers will earn the same level of compensation for the same level of effort in the prior year.
Figure 2 shows how a provider’s compensation rate can be adjusted to match each of the above philosophies.
The approach applied to a provider, service line, or entire organization depends on a variety of factors including strength of current rates, market benchmarks, the organization’s financial strength, and the competitive landscape. As shown in Figure 3, HSG’s survey respondents had significant variation in their organizational philosophy when implementing the updated MPFS. 28% of respondents were implementing the new rates with the intention of keeping compensation levels neutral and 24% have no intention of making any adjustments.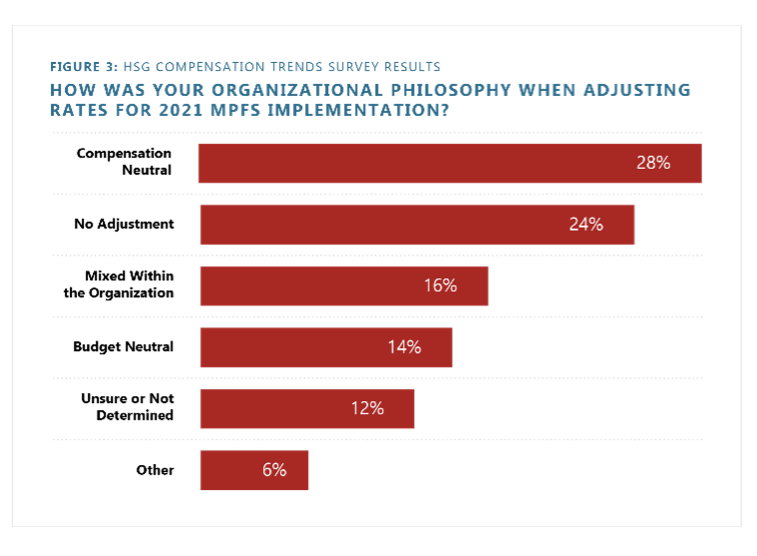
While provider compensation is never simple, the next few years will be increasingly complicated as organizations adjust compensation parameters to adapt to the new MPFS. Failure to address this issue could significantly threaten financial sustainability and/or provider satisfaction. Avoid these pitfalls and contact HSG to support your leaders in developing your strategy for MPFS transition.


