May / June Clinical Leadership & Infection Control Issue
May / June Clinical Leadership & Infection Control Issue
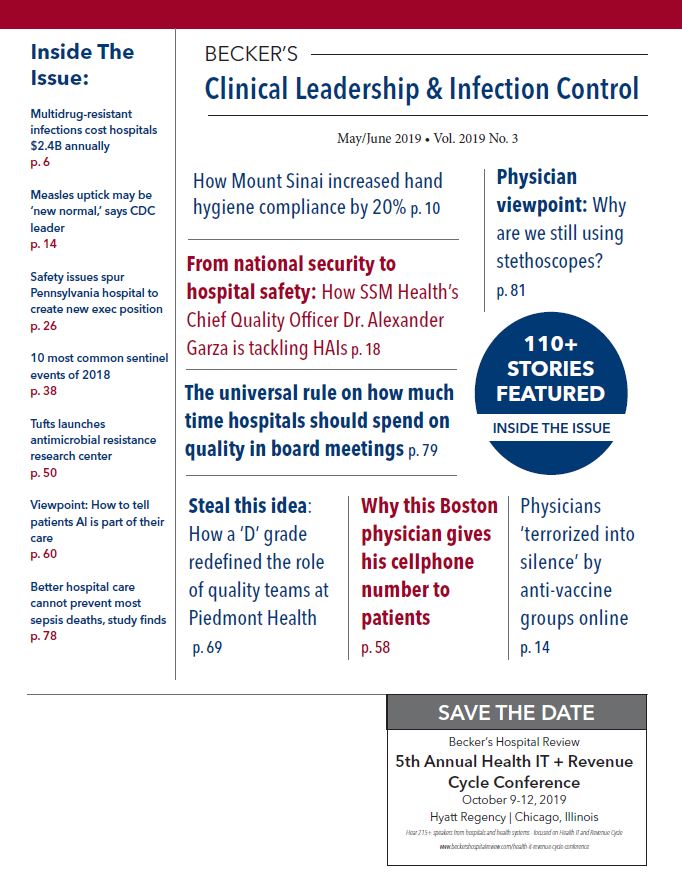
INFECTION CONTROL
Multidrug-resistant infections cost hospitals $2.4B annually
Hospitals spend more than $2 billion annually to treat patients with multidrug-resistant infections, according to a study published in Health Services Research. CLICK TO CONTINUE
How some hospitals, nursing homes are teaming up against antibiotic-resistant infections
Hospitals and nursing homes in Illinois and California are bathing patients in the antibacterial soap chlorhexidine as part of two CDC-funded studies to decrease antibiotic-resistant infections, reported NPR. CLICK TO CONTINUE
HAIs decreased in 2017, CDC report finds
Healthcare-associated infections decreased in the U.S.between 2016 and 2017, according to the CDC’s National and State HAI Progress Report. CLICK TO CONTINUE
NIH researchers call for more research into rare, polio-like illness
More research must be done to better understand acute flaccid myelitis, three researchers from the National Institutes of Health wrote in an op-ed published in Clinical Science and Epidemiology. CLICK TO CONTINUE
There are 4 types of anti-vaccine messages, study finds
A study published in Vaccine found that anti-vaccination discourse doesn’t always center on autism, and instead has four distinct themes. CLICK TO CONTINUE
Instagram, GoFundMe crack down on anti-vaccine content
Instagram and GoFundMe are among the latest social media companies to address anti-vaccine content online. CLICK TO CONTINUE
Undiagnosed, untreated HIV patients responsible for 81% of new transmissions
Individuals who didn’t know they had HIV or knew but were not receiving care accounted for 81 percent of HIV transmissions in 2016, according to CDC data released March 18. CLICK TO CONTINUE
How Mount Sinai increased hand hygiene compliance by 20%
New York City-based Mount Sinai Health System improved hand hygiene compliance 20 percent after implementing The Joint Commission’s Targeted Solutions Tool for Hand Hygiene, according to a blog post on the accrediting body’s website. CLICK TO CONTINUE
WHO's recommendations for 2019-20 flu vaccine: 3 notes
The World Health Organization finalized its recommendations for the composition of the 2019-20 flu vaccine March 21. CLICK TO CONTINUE
Delaying flu shots until October could prevent 22K illnesses, study finds
Fall is the best time to start vaccinating people against the flu, according to a study published in the American Journal of Preventive Medicine. CLICK TO CONTINUE
Kentucky governor says he purposely exposed children to chickenpox
Kentucky Gov.Matt Bevin said during a radio interview March 19 that he intentionally exposed his nine children to the chickenpox virus so they would contract the disease and gain immunity, according to the Courier-Journal. CLICK TO CONTINUE
NIH launches 1st clinical trial of universal flu vaccine
The National Institute of Allergy and Infectious Diseases, part of the National Institutes of Health, started the first clinical trial of a new universal influenza vaccine candidate. CLICK TO CONTINUE
Physicians ‘terrorized into silence’ by anti-vaccine groups online
Many physicians face online harassment when posting about vaccines on their practices’ social media pages, which can often scare them into silence, reported the Los Angeles Times. CLICK TO CONTINUE
50%+ of hospital trainees work while experiencing flu-like illness
Working while sick with influenza-like illness may be common in training programs at hospitals, according to a study published in the American Journal of Infection Control. CLICK TO CONTINUE
Measles uptick may be ‘new normal,’ says CDC leader
The U.S.will more regularly see measles outbreaks in pockets of unvaccinated individuals, health experts told STAT. CLICK TO CONTINUE
Rates of stethoscope cleaning, hand hygiene practices ‘lower than expected’ in ED, study says
A study published in the American Journal of Infection Control examined stethoscope cleaning and hand hygiene in an emergency department setting. CLICK TO CONTINUE
Flu shot, spray OK for next season, says American Academy of Pediatrics
Both the flu shot and nasal spray vaccine are acceptable for children during the 2019-20 flu season, the American Academy of Pediatrics announced March 14. CLICK TO CONTINUE
AMA calls on tech CEOs to address anti-vaccine content
The American Medical Association is calling on major technology companies to ensure their users have access to accurate information on vaccines. CLICK TO CONTINUE
Alexander Garza, MD, chief quality officer at St. Louis-based SSM Health, is no stranger to infectious disease prevention and response. CLICK TO CONTINUE
Nearly 40% of healthcare workers make errors when removing personal protective equipment
Mistakes in putting on or taking off personal protective equipment put healthcare workers at risk of contamination with multidrug-resistant organisms, according to a study published in Infection Control & Hospital Epidemiology. CLICK TO CONTINUE
CDC: 119,000+ US residents contracted staph in 2017, as progress to stem it slows
Bloodstream Staphylococcus aureus infections are still a threat in the U.S., and after early success in reducing serious staph infection rates, progress has slowed, according to a Vital Signs report released by the CDC. CLICK TO CONTINUE
How NorthShore University HealthSystem keeps CAUTI rates low
Evanston, Ill.-based NorthShore University HealthSystem significantly reduced its rate of catheter-associated urinary tract infections between 2012 and 2015, according to a case study from the Agency for Healthcare Research and Quality. CLICK TO CONTINUE
Matching subsidies for infection control effective at lowering HAI levels
Incentivizing infection control via subsidies could help encourage regional spending on healthcare infection control activities, according to a paper published in the Proceedings of the National Academy of Science. CLICK TO CONTINUE
WHO head: Next flu pandemic is matter of when, not if
A global flu pandemic is a realistic threat the world must prepare for, the World Health Organization said March 11. CLICK TO CONTINUE
Measles cases hit highest level since 2000
The CDC reported 764 measles cases as of May 3, which marks the highest annual total since U.S. health officials declared the disease eradicated in 2000. CLICK TO CONTINUE
Algorithm identifies patients at higher risk for hospital-acquired pneumonia
A new data-driven algorithm can identify patients at an increased risk for hospital-acquired pneumonia and ventilator-associated pneumonia and describe characteristics of carbapenem resistance in this population, a study published in CHEST Journal found. CLICK TO CONTINUE
Electronic hand hygiene system fails to improve ICU staff satisfaction
A study published in Antimicrobial Resistance & Infection Control examined the effect of introducing an electronic hand hygiene surveillance and intervention system into an intensive care unit. CLICK TO CONTINUE
14% of new hospital patients harbor superbugs: 4 study findings
Some hospital patients contain antibiotic-resistant bacteria on their hands or nostrils at the start of a hospital stay, which highlights the need for patient hand-hygiene programs, according to a study published in Clinical Infectious Diseases. CLICK TO CONTINUE
Daily antiseptic bath cuts infections 31% for patients with indwelling devices, study finds
A bacterial decolonization strategy involving daily bathing with an antiseptic soap can significantly reduce bloodstream infections in patients with catheters or lumbar drains, according to a study published in The Lancet. CLICK TO CONTINUE
Delaying flu shots until October could prevent 22K illnesses
Fall is the best time to start vaccinating people against the flu, according to a study published in the American Journal of Preventive Medicine. CLICK TO CONTINUE
State-mandated reporting laws may lower time spent on infection control activities
A study published in the American Journal of Infection Control examined the perceived impact of state-mandated healthcare-associated infection laws on infection prevention and control departments. CLICK TO CONTINUE
PATIENT SAFETY
Safety issues spur Pennsylvania hospital to create new exec position
Lancaster (Pa.) General Hospital created a new executive position to oversee clinical operations after a patient left the hospital wearing staff scrubs and was found wandering across town last fall, according to LancasterOnline. CLICK TO CONTINUE
Missouri hospital retains Medicare contract after colonoscopy death investigation
Harrisonville, Mo.-based Cass Regional Medical Center is no longer at risk of losing its Medicare contract, according to The Kansas City Star. CLICK TO CONTINUE
E-prescribing systems could increase medication error risk
Implementing electronic prescribing and medication administration systems in hospitals could increase overall medication risk, according to a study published in BMC Health Services Research. CLICK TO CONTINUE
Stop calling physicians ‘second victim’ of medical errors, patient advocates say
The medical community should stop referring to physicians as the “second victim” of a medical error, four patient safety advocates wrote in an editorial for The BMJ. CLICK TO CONTINUE
Johns Hopkins All Children’s dodges millions of dollars in fines for safety issues
State regulators could’ve fined St.Petersburg, Fla.-based Johns Hopkins All Children’s Hospital millions of dollars for failing to report numerous incidents of patient harm.Instead, they slapped the hospital with a $4,500 fine, reported the Tampa Bay Times. CLICK TO CONTINUE
Study: Longer resident shifts don’t threaten patient safety
A study published in The New England Journal of Medicine examined whether long shifts during medical residencies adversely affect patient safety. CLICK TO CONTINUE
CMS updates immediate jeopardy citation guidelines
CMS revised its guidance for surveyors related to identifying immediate jeopardy cases in March. CLICK TO CONTINUE
Overlapping surgery is safe, except for high-risk patients: 4 study findings
Concurrent surgeries in which a surgeon runs two operations at once are not significantly associated with higher patient mortality or complication rates for most patients, according to a study published Feb.26 in JAMA. CLICK TO CONTINUE
Employee engagement is crucial for patient-centered care, says Press Ganey
Employee alignment and engagement is crucial for health systems seeking to build an organizational structure that supports patient-centered care, according to Press Ganey’s 2019 Strategic Insights report, titled “Accelerating Transformation: Translating Strategy Into Action.” CLICK TO CONTINUE
At least five patients who died under the care of a former physician at Columbus, Ohio-based Mount Carmel Health System may have survived if they had received the correct treatment, health system officials told The Columbus Dispatch. CLICK TO CONTINUE
48 Mount Carmel nurses, pharmacists under review amid patient deaths
Forty-eight former and current employees at Columbus, Ohio-based Mount Carmel Health System are under review as part of an internal investigation after allegations that a physician ordered fatal doses of pain medication for nearly three dozen patients. CLICK TO CONTINUE
Serious medical errors rise in Minnesota: 4 findings
Minnesota hospitals and licensed surgery centers reported 384 medical errors in 2018, marking an increase from the 342 errors tallied a year prior, according to the state health department’s 15th annual adverse event report published March 1. CLICK TO CONTINUE
U of Illinois at Chicago overlooked serious issues with clinical trial, documents show
University of Illinois at Chicago has publicly denied its failure to oversee a troubled clinical trial involving adolescents, but newly obtained documents show the university did acknowledge some shortfalls to federal investigators, according to an investigative report from ProPublica Illinois. CLICK TO CONTINUE
Internal FDA database hides dangerous device malfunctions from physicians, KHN report finds
The FDA permits some devicemakers to file reports on device-related injuries and malfunctions in a discreet database that is not accessible to physicians or the general public, according to an investigation from Kaiser Health News. CLICK TO CONTINUE
Retained guidewires still a ‘significant patient safety issue’
A study published in The Joint Commission Journal on Quality and Patient Safety examined reports of unintentionally retained guidewires to ascertain the threat to patient safety. CLICK TO CONTINUE
CMS faults New Jersey nursing home for outbreak that killed 11 kids
State health inspectors initially blamed poor hygiene for an adenovirus outbreak that killed 11 kids at a Wanaque, N.J., nursing home and rehab center last fall, but a CMS report found the bigger problem was that the facility’s leaders didn’t respond fast enough when the outbreak hit, according to northjersey.com. CLICK TO CONTINUE
Study: Diagnostic accuracy improves with ‘collective intelligence’
When diagnoses from a group of physicians are combined, they are more accurate than a single diagnosis — even when the group may not have specialty expertise, according to a study published March 1 in JAMA. CLICK TO CONTINUE
Patient dies after fight at Florida healthcare facility
Police are investigating the death of an elderly man who died after getting into a fight with another patient at a long-term care facility in Florida, reported News4Jax. CLICK TO CONTINUE
Vanderbilt hit with $25.5M suit over wrong-site surgery
A Tennessee woman filed a lawsuit against Nashville-based Vanderbilt University Medical Center March 19, claiming surgeons operated on her wrong kidney, reported The Tennessean. CLICK TO CONTINUE
Surgical staplers linked to 41,000 injury, malfunction reports, FDA says
The FDA is warning healthcare providers about the risk of serious injury, malfunction and death associated with surgical staplers and implantable surgical staples. CLICK TO CONTINUE
10 most common sentinel events of 2018
Patient falls were the most frequently reported sentinel event in 2018, according to a March 13 report from The Joint Commission. CLICK TO CONTINUE
Clinicians delayed CPR on patient who died at New Jersey hospital, CMS finds
A CMS investigation revealed clinicians at Winslow Township, N.J.-based Ancora Psychiatric Hospital failed to start CPR for eight minutes on an unconscious patient who ultimately died, according to the Courier Post. CLICK TO CONTINUE
Customized drug alerts protect patients from medication errors, study finds
Researchers from Memphis, Tenn.-based St. Jude Children’s Research Hospital used a comprehensive method to reduce drug interaction alerts clinicians receive, improving EHRs to lower alert fatigue and boost patient safety, according to a study published in Pediatrics. CLICK TO CONTINUE
CDC's secrecy of drug-resistant outbreaks in hospitals sparks patient safety debate
Hospitals and federal agencies often keep outbreaks of drug-resistant infections quiet from the public, which could pose a threat to patient safety, reported The New York Times. CLICK TO CONTINUE
10 top patient safety concerns for 2019, ranked by ECRI Institute
Using EHRs to communicate diagnoses and manage test results earned the No. 1 spot on ECRI Institute’s list of the Top 10 Patient Safety Concerns for 2019. CLICK TO CONTINUE
Baylor St. Luke’s pledges reforms after medical error leads to patient death
A CMS inspection revealed staff at Houston-based Baylor St.Luke’s Medical Center made more than 100 mistakes in labeling blood during a four-month period, according to the Houston Chronicle. CLICK TO CONTINUE
FDA warns against robotic surgery for cancer due to safety concerns
The FDA on Feb.28 issued a warning for providers regarding the use of robotically-assisted surgical devices for mastectomies and other cancer surgeries. CLICK TO CONTINUE
ANTIBIOTIC RESISTANCE & STEWARDSHIP
Facility type affects antibiotic stewardship guideline adherence
A study published in Antimicrobial Resistance & Infection Control found that lower complexity facilities continue antibiotic therapy longer than guidelines recommend. CLICK TO CONTINUE
Drug-resistant infections to kill 1,328% more people annually by 2050, UN warns
Drug-resistant infections will kill 10 million people annually by 2050 if the world does not take more action to address antibiotic resistance now, the United Nations said in a report released April 29. CLICK TO CONTINUE
Researchers pinpoint mechanism that makes bacteria resistant to antibiotics
Physicists at McMaster University in Ontario, Canada, identified a simple mechanism deadly bacteria use to fend off antibiotics, a study published in Nature Communications Biology found. CLICK TO CONTINUE
Over 5-year period, antimicrobial stewardship programs saved US hospitals $732 per patient
A study published in Antimicrobial Resistance & Infection Control examined the economic and clinical impact of antimicrobial stewardship programs. CLICK TO CONTINUE
Antibiotic, PPI use may increase pediatric C. diff risk
Children using antibiotics and/or proton pump inhibitors face a higher risk of developing Clostridioides difficile infection, according to a study published in Infection Control & Hospital Epidemiology. CLICK TO CONTINUE
Shorter mechanical ventilation duration linked to timely antibiotic prescription in pediatric ICU
A study published in Pediatric Critical Care Medicine examined the effect of prescribing antibiotics at the onset of mechanical ventilation on clinical outcomes. CLICK TO CONTINUE
Antibacterial consumer products are fueling antibiotic resistance, study finds
The use of consumer products that contain the chemical triclosan is fueling antibiotic resistance, according to a study published in Antimicrobial Agents and Chemotherapy. CLICK TO CONTINUE
Decision tree, risk score methods effective predictors of drug-resistant infections
A study published in Infection Control & Hospital Epidemiology compared the use of logistic regression-derived risk scores and machine learning-derived decision trees for predicting multidrug-resistant gram-negative infections. CLICK TO CONTINUE
Researchers develop system to map out areas of antibiotic resistance
University of Wisconsin-Madison School of Pharmacy researchers designed a system that can map out antibiotic trends across the state. CLICK TO CONTINUE
Physicians more likely to receive antibiotic prescription training than nurses, pharmacists
Training and support related to antibiotic prescribing is lower among nurses and pharmacists than physicians, according to a study published in Antimicrobial Resistance & Infection Control. CLICK TO CONTINUE
Tufts launches antimicrobial resistance research center
Boston-based Tufts Medical Center and Medford, Mass.-based Tufts University created a center dedicated to fighting antimicrobial resistance, the entities announced March 7. CLICK TO CONTINUE
Pediatric telemedicine visits may lead to uptick in antibiotic overprescribing
Pediatric patients were more often prescribed antibiotics during direct-to-consumer telemedicine visits than during in-person urgent care or primary care appointments, according to research published in Pediatrics. CLICK TO CONTINUE
5 ways bedside nurses can improve antibiotic stewardship
Ensuring bedside nurses are integrated into antibiotic stewardship activities can help those activities be successful, according to a study published in Infection Control and Hospital Epidemiology. CLICK TO CONTINUE
Patient privacy curtains often contaminated with superbugs, study finds
Contamination of patient privacy curtains with multidrug-resistant organisms is common, according to a study presented at the European Congress of Clinical Microbiology and Infectious Diseases meeting in Amsterdam, Netherlands, April 13 through April 16. CLICK TO CONTINUE
Nearly 70% of pediatric caregivers work around programs to cut antibiotic resistance, survey finds
While most providers believe that programs aiming to reduce the threat of antimicrobial resistance can improve pediatric care, many admit they use workarounds from time to time, according to survey results published in Infection Control & Hospital Epidemiology. CLICK TO CONTINUE
Highly resistant E. coli strain found in NYC hospital patients
EResearchers identified a highly resistant strain of E. coli in four patients at a hospital in New York City, according to a study published in Antimicrobial Agents and Chemotherapy. CLICK TO CONTINUE
54% of children with community-associated C. diff recently used antibiotics, study shows
A study published in Epidemiology & Infection found recent antibiotic use was strongly linked to the onset of community-associated Clostridioides difficile infections in young children. CLICK TO CONTINUE
PATIENT EXPERIENCE
Physician viewpoint: How pizza and coffee helped me see patients in new light
Understanding that patients have challenges that make it hard to prioritize health can help physicians connect with them and provide better care, a physician wrote in a piece on Philly.com. CLICK TO CONTINUE
Viewpoint: Why physicians should embrace tears
Crying is often seen as an “extreme emotional behavior” that is frowned upon in the medical world, according to Jalal Baig, MD, a hematology/ oncology physician at the University of Illinois at Chicago. CLICK TO CONTINUE
Immersive VR experience helps calm pediatric ICU patients, study finds
A fully immersive virtual entertainment experience can help calm patients in the pediatric intensive care unit, according to a study published in Pediatric Critical Care Medicine. CLICK TO CONTINUE
3 tips for talking to terminal patients about end-of-life care
Oncologists should have open conversations with terminal cancer patients about their prognosis and end-of-life care to help reduce symptoms of anxiety and depression, according to an editorial published in JAMA Oncology. CLICK TO CONTINUE
How noncompete clauses can sever patient-provider relationships
Noncompete clauses, which are becoming more common in healthcare, can often drive a wedge between providers and their patients, reported The New York Times. CLICK TO CONTINUE
Why this Boston physician gives his cellphone number to patients
Clement Bottino, MD, a pediatrician at Boston Children’s Hospital, has given his cellphone number to patients since he started his practice in 2009. CLICK TO CONTINUE
Viewpoint: How to tell patients AI is part of their care
A s artificial intelligence use expands in the healthcare space, physicians must be aware of how to properly explain the role of AI to patients and address ethical concerns that arise, a commentary published in the American Medical Association’s Journal of Ethics said. CLICK TO CONTINUE
Illinois nurses canoe to hospice patients' homes amid flooding
Some Illinois nurses waded through floodwaters and canoed to hospice patients’ homes in April after the Mississippi River flooded some areas of the Quad Cities, reported WQAD News 8. CLICK TO CONTINUE
Banner Health launches podcast featuring medical stories
Phoenix-based Banner Health has launched a podcast called “Bedside Stories” to give listeners the opportunity to hear some of the most engaging stories of patients and clinicians at the system. CLICK TO CONTINUE
AI teaches physicians to be more empathetic
Hospitals are now adopting artificial intelligence tools to teach physicians and staff to be more empathetic toward patients and families, according to The Wall Street Journal. CLICK TO CONTINUE
AHRQ launches app to improve patient engagement
The Agency for Healthcare Research and Quality debuted a mobile application that helps patients prepare for medical visits. CLICK TO CONTINUE
Airbnb expands medical stay program: 4 things to know
Airbnb expanded its Open Homes program for medical stays through two new partnerships, the company announced March 26. CLICK TO CONTINUE
Having a medical professional in the family ups likelihood of hitting 80
Having a nurse or physician in your family can result in a longer life, among other benefits, according to a working paper released by the National Bureau of Economic Research and authored by researchers from Stanford (Calif.) Medicine. CLICK TO CONTINUE
Viewpoint: When families don’t respect nurses, patient care can suffer
Patients and their families often place more weight on a physician’s words than a nurse’s, which can threaten care quality, a registered nurse of 14 years wrote in an article for Healthline’s Anonymous Nurse column. CLICK TO CONTINUE
3 factors affecting patient handoff communication
A study published in Journal of General Internal Medicine examined complex interactions and communication norms that shape face-to-face patient handoffs. CLICK TO CONTINUE
Costly, aggressive treatments often used on end-stage cancer patients
Many patients with late-stage cancers pursue aggressive treatment options instead of end-of-life care, according to a study published in JNCI Cancer Spectrum. CLICK TO CONTINUE
1st-year physicians spend more time interacting with EHRs than patients
First-year physicians spend, on average, 43 percent of the day interacting with patients' EHRs, according to a study published in JAMA Internal Medicine. CLICK TO CONTINUE
Physician viewpoint: Lack of EHR sharing prevents patient care
Patients suffer treatment delays and are sometimes forced to undergo medical tests they have already completed when they switch providers, infectious diseases specialist Pranay Sinha, MD, wrote in WBUR. CLICK TO CONTINUE
QUALITY IMPROVEMENT & MEASUREMENT
Steal this idea: How a ‘D’ grade redefined the role of quality teams at Piedmont Health
Leigh Hamby, MD, CMO of Atlanta-based Piedmont Health, thought his system was effectively executing quality initiatives when a surprising Leapfrog rating shook the status quo. Suddenly, he realized his team needed to reexamine their understanding of quality. CLICK TO CONTINUE
Ohio lawmakers call for stricter hospital regulations after Mount Carmel deaths
Some Ohio lawmakers are calling for increased hospital oversight in the wake of a patient death investigation at Mount Carmel West hospital in Columbus, Ohio, reported The Columbus Dispatch. CLICK TO CONTINUE
Leapfrog CEO: CMS’ readmission reduction program is imperfect, but effective
Critics of CMS’ Hospital Readmission Reduction Program are often quick to point out its flaws. CLICK TO CONTINUE
Patient gratitude can positively affect care team performance
Gratitude from patients has a significantly positive effect on the performance of a medical team, according to a study published in Pediatrics. CLICK TO CONTINUE
5 most challenging Joint Commission requirements for hospitals in 2018
The Joint Commission listed the maintenance of fire protection systems as the requirement most often identified as “not compliant” during surveys and reviews at hospitals in 2018. CLICK TO CONTINUE
Flu vaccine may help lower death risk among heart failure patients, study finds
A study published in Open Forum Infectious Diseases found that the influenza vaccine could affect mortality rates among patients with heart failure. CLICK TO CONTINUE
NAHQ creates framework for healthcare quality teams: 3 things to know
The National Association for Healthcare Quality created a framework outlining key competencies for healthcare quality teams. CLICK TO CONTINUE
Surgical outcomes vary across health systems with top hospitals, study finds
Surgical outcomes vary significantly across health systems that include some of the country’s highest-rated hospitals, according to a study published March 13 in JAMA Surgery. CLICK TO CONTINUE
AHA weighs in on proposed star ratings changes: 4 things to know
The American Hospital Association offered input on potential changes to CMS’ Overall Hospital Star Ratings mythology in a March 27 comment letter to Kate Goodrich, MD, CMO of CMS. CLICK TO CONTINUE
CMS push to curb HACs dings level 1 trauma centers, says Carilion’s quality chief
CMS’ Hospital-Acquired Condition Reduction Program offers a narrow view into the quality and safety at level 1 trauma centers, Jonathan Gleason, MD, chief quality officer for Roanoke, Va.-based Carilion Clinic, told WDBJ 7. CLICK TO CONTINUE
CMS star ratings don’t account for surgical volumes, study finds
CMS does not adequately assess the effect of surgery volume when calculating its Overall Hospital Quality Star Ratings, according to a study published in JBJS Open Access. CLICK TO CONTINUE
Hospital-associated sepsis on decline, but treatment costs climb by $1.5B
While hospitals are doing a better job of preventing and treating sepsis, patients who develop the infection are becoming sicker. CLICK TO CONTINUE
Colorado 2nd state to enact law on surgical smoke in OR
Colorado is the second state in the U.S.to adopt a surgical smoke evacuation law to protect perioperative nurses and surgical team members. CLICK TO CONTINUE
Accounting for social risk factors can help safety-net hospitals avoid readmission penalties
Social risk factors, such as poverty, can affect readmissions to safety-net hospitals, thereby affecting federal penalties for readmission rates, according to a study published in Health Services Research. CLICK TO CONTINUE
Nurses’ work environments affect patient outcomes, study finds
The state of a nurse’s work environment can affect nursing care quality, job satisfaction and patient outcomes, according to a study published in Medical Care. CLICK TO CONTINUE
100+ hospitals have childbirth complication rates 2 times above norm, USA Today investigation finds
At least 120 hospitals nationwide have childbirth complication rates that are two times higher than other hospitals, according to an investigative report from USA Today. CLICK TO CONTINUE
San Antonio hospital makes changes to heart program after low Society of Thoracic Surgeons score
After being ranked as one of the lowest performing hospitals in the country for adult heart surgeries in August 2018, University Hospital in San Antonio is retooling its heart care program, according to San Antonio Express-News. CLICK TO CONTINUE
Better hospital care cannot prevent most sepsis deaths, study finds
Sepsis is the leading cause of death in U.S. hospitals, but improved hospital care alone may not be enough to prevent the deadly condition, according to a study published in JAMA Network Open. CLICK TO CONTINUE
Stricter rules for accrediting bodies met with industry debate
Healthcare organizations are split on whether the White House should impose stricter regulations on healthcare accreditation bodies to limit conflicts of interest, reported The Wall Street Journal. CLICK TO CONTINUE
How Barnes-Jewish Hospital cut unnecessary UTI testing in half
A simple change to St.Louis-based Barnes-Jewish Hospital’s electronic ordering system helped cut the number of unnecessary urine culture tests ordered for suspected urinary tract infections nearly in half, according to a study published Feb.21 in Infection Control and Hospital Epidemiology. CLICK TO CONTINUE
The universal rule on how much time hospitals should spend on quality in board meetings
Board engagement is crucial for healthcare organizations seeking to create cultures of safety and quality. CLICK TO CONTINUE
Nurse navigators linked to fewer readmissions, deaths among heart attack patients
A program in which nurse navigators help heart attack patients transition from hospital to outpatient care can help lower readmission and mortality rates, according to research presented at the American College of Cardiology’s Cardiovascular Summit in Orlando. CLICK TO CONTINUE
Patient deaths after colorectal surgery declined from 2008-17
The rate of adults who died within 30 days of colorectal surgery dropped from 4.3 percent in 2008 to 2.9 percent in 2017, according to the Agency for Healthcare Research and Quality’s Patient Safety Chartbook. CLICK TO CONTINUE
How Kaiser Permanente used new assessment criteria to reduce admissions
Emergency physicians at Oakland, Calif.-based Kaiser Permanente hospitals reduced admissions and cardiac stress testing by using new criteria to assess chest pain patients’ risk for subsequent cardiac events, according to an article published in Annals of Emergency Medicine. CLICK TO CONTINUE
Text message system may improve patient outcomes after surgery, study finds
For patients who had a total hip or knee arthroplasty procedure, using a text-messaging service bot for patient education may improve clinical outcomes, a study published in The Journal of Bone and Joint Surgery found. CLICK TO CONTINUE
Physician viewpoint: Why are we still using stethoscopes?
The stethoscope — invented in 1816 — is long overdue for a redesign, according to Davinder Ramsingh, MD, an anesthesiologist at Loma Linda (Calif.) University Medical Center. CLICK TO CONTINUE