Artificial Intelligence-supported digital applications (AI applications) are expected to transform radiology. With more than 300 AI applications cleared by the FDA, they have a broad range of use cases in radiology1. AI applications for image interpretation are generating excitement within radiology with potential to aid in image processing and interpretation with greater accuracy and sensitivity. In addition, non-interpretative AI applications have the potential to play important roles in improving efficiency, safety, and quality.
Despite the promise AI applications hold in radiology, the question about who will pay is critical for ensuring adoption. Today, only six out of the 300+ regulatory-approved AI applications in radiology are reimbursed worldwide. Healthcare systems need to find the right balance when determining which AI applications to pay for and which AI applications not to. Reimbursement pathways are complicated and payers admit that this can be challenging2.
For some radiology AI applications, the benefits of the application may sufficiently serve as the incentive. For others, payers may have to consider reimbursing the AI application separate from the cost of the underlying imaging studies. In such circumstances, it is important for payers to develop a clear set of criteria to decide which AI applications should be paid for separately.
This lack of public funding is a significant obstacle for advancing AI in radiology and could delay the realization of AI’s full potential in improving patient care, according to Franziska Lobig, Access Lead for Radiology at Bayer AG and one of the authors of To Pay or Not to Pay for Artificial Intelligence Applications in Radiology. Other experts agree that time is crucial for developing a framework for reimbursement. Dr. Ankur Sharma, Head of Medical Affairs for Digital Radiology at Bayer, said the lack of standardized reimbursement inhibits progress, stifles innovation, and prevents patients from accessing advanced diagnostic technologies. He added that action is needed to establish a comprehensive reimbursement framework that incentivizes investment in companies and technology to ensure patients receive the highest quality care available.
Fig. 1: Availability of Supporting Evidence vs. Nature of Benefit
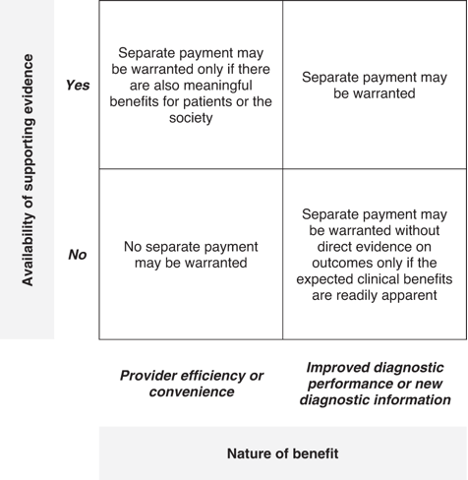
The authors of this paper propose the following framework when deciding which products should receive reimbursement. The framework proposed two aspects to consider for determining reimbursement of radiology AI applications: nature of benefits and availability of evidence. As radiology AI applications are heterogeneous, they offer a range of benefits to different stakeholders. Applications that solely improve efficiency may not require additional payment as providers have incentives to adopt them. For example, an app that is a de-noising algorithm and can reduce scan time, may not need separate reimbursement. However, other quadrants are for improved diagnostic performance or new diagnostic information. The benefit of these AI applications is primarily to the healthcare system and patient rather than the provider. They would need separate reimbursement since providers may not have the incentive to adopt them, but they bring large societal benefits.
With the proposed framework payers would need to consider several important issues before determining their payment policies for radiology AI applications. First, payers would have to define what constitutes a meaningful benefit – as opposed to just a statistically significant improvement – and what the minimum level of evidence is to support the existence of such a benefit. Valuing healthcare interventions can be complex, and radiology AI applications are no different. Cost-offsets may be easy to quantify, but the value of an earlier or more accurate diagnosis may be much harder to value.
Improving diagnosis may increase total healthcare costs by increasing downstream spend on additional investigations or treatments, and therefore, payers may have to consider not just the value, but also potential budget impact.
In addition, the value of an AI application may differ substantially between healthcare systems, and therefore, payers will have to evaluate radiology AI applications within the context of their own healthcare systems and determine whether and how to pay for these applications. For example, in a healthcare system with poor access to specialist radiologists, a radiology AI application may help improve diagnostic accuracy and clinical outcomes, whereas in a healthcare system with good access to specialist radiologists the same application may help improve efficiency of the reporting radiologist more than diagnostic accuracy.
Changing how we think about new technologies and payments is important to anyone who wants to improve patient care and push for further overall healthcare innovation, said Dr. Sharma. Reconstructing the future of radiology reimbursement can lead to tremendous benefits for patients, radiologists, and the healthcare system.
To learn more and watch the recent webinar, go to Calantic | Resources.
References
1. American College of Radiology. ACR Data Science Institute AI Central. https://aicentral.acrdsi.org/ (2022).
2. Centre for Medicare and Medicaid Services. Hospital Outpatient Prospective Payment and Ambulatory Surgical Center Payment Systems and Quality Reporting Programs - Proposed rule 2023. 87, 71748–72310 (2022).


