The healthcare system is faced with a tsunami of incoming data. In fact, the average hospital produces roughly 50 petabytes of data every year. That's more than twice the amount of data housed in the Library of Congress and amounts to137 terabytes per day.
Healthcare data generation is increasing each year by nearly 50%, which complicates how pertinent information is integrated and managed across clinical, administrative and financial systems. The health insurance industry has its own unique set of data challenges, which have recently increased the demand for interoperability, bidirectional data exchange and an overall modernization of data infrastructure.
Patient data is often dispersed across multiple, disconnected systems, which obstructs a holistic and longitudinal view of their health journey and status. In addition, key datasets that are proven to positively contribute to patient engagement and clinical outcomes are often missing. These include social determinants of health (SDoH); lifestyle; behaviors such as sleep, nutrition or physical activity; and patients’ personal preferences for communication.
A unified data model is a standardized scheme structure that uses shared data language and concepts across the organization. It enables visibility into all collected data points to facilitate a comprehensive understanding of the entire data narrative. Unified data models alleviate many of the current challenges payers and providers are facing and work best when they reside within a connected digital ecosystem that orchestrates all data sources into common tables and schemas to fulfill the vision for care management of the future.
In this blog, we highlight the need for a unified data model for patients, providers and payers. We also address how to get started in building a unified data model.
Benefits to patients
Most patients have multiple channels through which they receive health care and service, which means they likely have medical data and records that reside across numerous data repositories. We know it is better — for patients, providers and payers — to see a comprehensive dataset that includes all healthcare information, including medical history, social risks, laboratory results, diagnostics, medications, care episodes, insurance coverage, etc.
Longitudinal health records are an essential step, but more can be done to better integrate and manage data across the entire health ecosystem. Unified data means, for example, having the data access and ability to triangulate insights related to acute medical needs with social risks and utilization patterns — all in an effort to avoid unnecessary hospitalizations and deliver services that are most essential to the patient.
Benefits to providers
A unified data model — a comprehensive patient record that includes data from various sources throughout the healthcare system — can improve quality of care, maintain efficient and cost-effective patient records, and help healthcare providers keep costs down. A recent report by the American Hospital Association Center for Health Innovation emphasized the need to integrate all sources of data types beyond clinical information in medical records. (Leveraging Data for Health Care Innovation, January 2021.)
Data within a connected ecosystem leads to better clinical decision support through the use of intelligent workflows, automation of non-clinical tasks, touchless care planning, and integrated care and service. Unified data can also lead to reduced errors by standardizing data formats and reducing the need for manual data entry.
Creating unified data records is an achievable goal, but it will require some investment in the underlying infrastructure and prioritization of advancing digital maturity to create new insights, solve business problems, increase revenue and decrease costs. Hospitalizations, doctors’ visits, nursing home care, in-home care, telehealth, networks and targeted marketing campaigns can all benefit from a unified model.
Benefits to payers
Unified data enables payers to better leverage member information across the entire value chain. Unified data sets that include holistic sources such as demographics, enrollment, clinical, social, behavioral and claims data can assist payers in delivering a whole-person model of care. Unified data models in a payer setting enable those interacting with members to do high-value tasks, such as set member appointments, determine benefit eligibility, coordinate and manage holistic care, and quickly surface claims information.
For example, when payers have a 360 degree view in their contact center, measurable improvements in member and end user experience can be achieved by reducing the average call handling time, improving the first call resolution and the overall quality of service. These improvements yield an overall return on investment of between 80% and 120% based on a recent PwC client engagement — all resulting from a well-designed contact center based on a unified data model.
Furthermore, a unified data model can unlock efficiencies that are scalable across the organization. Insights related to gaps in care, referral patterns, out of network utilization, medication adherence and more can be gleaned from having access to data across a patient's health record. When considering advanced risk adjustment capabilities, unified data models can bring a wide variety of risk factors and vulnerabilities into focus and bring about a more refined understanding of member risk. This can become a business differentiator for payers as they seek to cultivate cost-effective programs, while also providing top-tier care and customer service.
Getting Started: It’s a journey, not a sprint!
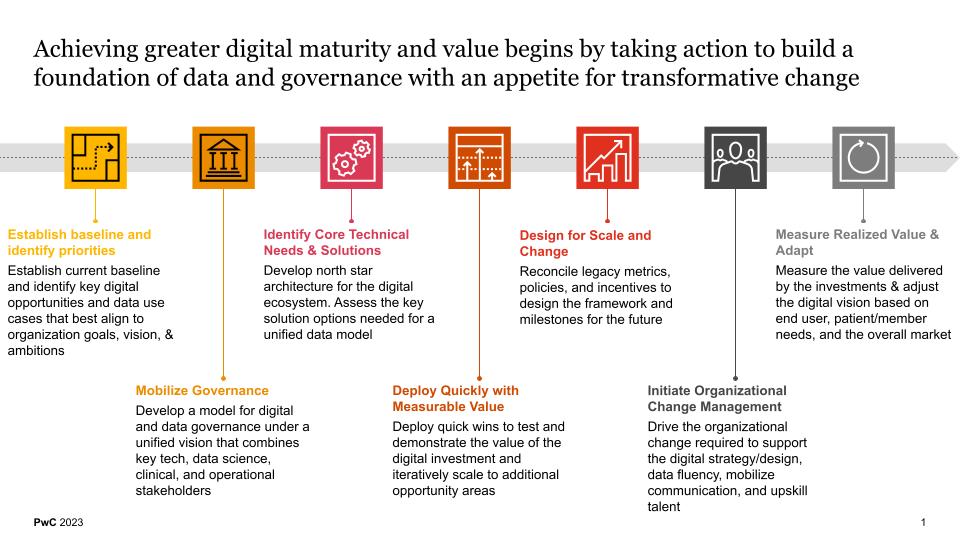
The pace of change in healthcare necessitates that organizations begin thinking about developing a unified data model within a connected digital ecosystem to drive effective digital transformation. The future leaders and innovators in healthcare will be those that can unlock their data, analyze it and integrate it into the day to day fabric of the organization so it can be acted upon. It’s important to begin by establishing a baseline understanding of where your organization is within its digital and data maturity evolution. From there, identify the set of priorities needed to advance capability maturity towards a modernized and transformed future state. After these level setting activities, applying some consideration to mobilizing digital governance is a good next step. This helps establish guard rails and clear lines of decision making authority and data asset ownership.
Next, identify core technical needs and solutions, and follow up by deploying quick wins to test and demonstrate the value of the digital investment. After that, spend some time designing your program for effective scalability and wide-scale change, then initiate the organizational change management program. Change management is an important component of the transformative journey and can often be the primary lever for success and sustainability. Finally, measure the value delivered by the digital and data investments and adjust based on patient needs and the overall market.
Digital and data maturity is needed to build an integrated, flexible and scalable ecosystem of capabilities that are aligned to the organizational strategy and rooted in the organization’s culture. It begins by creating a unified foundation of data assets that is liberated and leveraged against a set of clear priorities and governed with an appetite for transformative change.
Contact us to help you get started in building a unified data model and transforming digital health.


