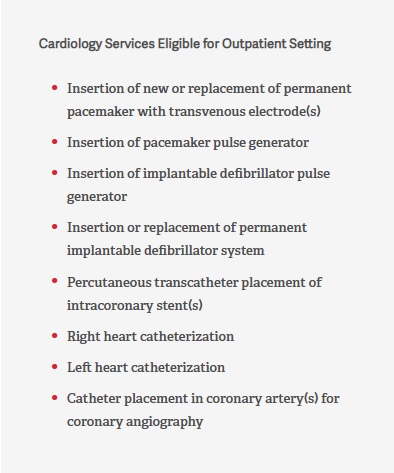
Over the past several years, CMS has continually expanded the list of services approved for delivery in an outpatient setting or office-based lab (OBL).
Given the savings CMS has seen from these moves, the nation’s largest payer will likely continue to enact policy and payment updates that shift cases to lower-cost settings. And with a growing list of cardiac procedures approved for ASCs and OBLs, facility leaders need to develop their service offerings. Moreover, CMS established reimbursement for many services at rates that make sense, creating a situation where providers can successfully perform cardiac procedures in outpatient settings.
Leadership of facilities interested in adding these new cardiac services to their operations should take the following steps to ensure future success:
- Cardiology- and cardiac-related outpatient procedural services remain an evolving specialty in the ASC setting. Before considering the addition of these services or establishment of a hybrid ASC or OBL, review current payer contracts to confirm these codes are included and that the existing reimbursement is appropriate.
- State regulations may impact the types of services allowed in an ASC or OBL. Validate which services are allowed in your state and confirm the community standards in your market. Since some states’ additional regulations may not follow Medicare, it is important to assess guidelines on all levels.
- Once state regulations have been confirmed, work with commercial and government payers to determine whether cardiology services performed in an ASC or OBL setting will be reimbursed. Medicare allows specific codes in each site of service, but commercial payers don’t always follow Medicare’s clinical or reimbursement guidelines and vary on which types of services they approve in each setting, market, and state
- When moving care from a hospital to a freestanding ASC or OBL, review the types of procedures and projected volume with the physicians. This data is critical to supporting the savings opportunity discussion with the payer.
- Present the expected savings to payers, with an opportunity to negotiate rates. The location will add complexity to contracting, and payers may have to create new methodologies for cardiac-related services in ASCs and OBLs.
- In order to ensure accurate and competitive rates, provide education on cardiac-specific services to payers that have not covered them previously.
- Commercial payers may need to determine how to reimburse based on the site of service if their existing reimbursement methodologies are not designed for traditionally inpatient or office-based services.
- If a procedure is moving from the hospital to an OBL or ASC, there may be an opportunity to negotiate a nonstandard rate greater than Medicare for managed Medicare patients.
- Medicare has allowed over a dozen procedural codes related to pacemaker placement and revision in ASCs, but these procedures are not approved and or reimbursed in the OBL setting.
- Peripheral vascular intervention and cardiac catherization procedure codes may be allowed in both the ASC and OBL settings if there are no state limitations. Be mindful that the site of service will impact the physician billing; OBLs are coded as place of service 11, which includes the professional compensation for the physician and the technical component for the facility (e.g., cath lab).
- If a physician performs the service in an ASC, the professional and ASC services are billed separately. The physician would send a separate invoice for their professional services, while the ASC would be paid for facility services.
As CMS expands the list of cardiology services that can be performed in outpatient settings, opportunities for ASCs and OBLs expand as well. But leaders must address these key considerations before their organizations can proceed. It is important to finalize these issues ahead of recruiting providers, purchasing capital equipment, and preparing the policies and procedural guidelines required to expand service offerings.


