The Keys to Care
Optimizing a healthcare organization’s staffing mix is rightly viewed as a way to boost efficiency and reduce costs. What may not be as immediately apparent is the connection between the efficient orchestration of talent and improvements in patient experience, satisfaction, and the quality of care they receive.
Let’s examine what can be done to improve the patient experience by enhancing the well-being of healthcare professionals. We believe the key rests in compassion and the science of talent planning.
Right Place, Right Time, Right Support
Improving the patient experience is a goal of every healthcare organization. But within that simple idea is an incredible amount of complexity.
When thinking about how to improve the patient experience, we need to take a step back and think about all the touchpoints of care, and what each of those look and feel like. Then, we take another step back and look at the processes needed to ensure a healthcare professional is at the right place at the right time to provide care. Take a final step back and we can start to see the culture behind the processes and whether those providing care are being cared for themselves and are receiving the support they need to be at their best.
Measuring the Patient Experience
The most tangible way of measuring the patient experience is through HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems). HCAHPS is a survey and data collection methodology for measuring patients’ perceptions of their experience. While many healthcare organizations conduct their own assessments and surveys, HCAHPS is the national standard of measurement and the only uniform tool available to make comparisons across hospitals locally, regionally, and nationally. CMS publishes HCAHPS results on the Care Compare website quarterly, with the oldest quarter of patient surveys rolling off as the most recent quarter rolls on.
Low HCAHPS scores negatively impact a hospital in two ways. First, as the information is public, low scores can hurt an organization’s reputation, making it harder to attract and retain both patients and healthcare professionals. Second, lower scores limit the amount of funding a hospital receives from Medicare.
Staffing and the Patient Experience
An article from Eastern Michigan University states that when healthcare facilities have insufficient nurses on staff, the welfare of patients can be compromised. Moreover, overwhelmed nurses can overlook details or not be able to fully engage with patients. This leaves patients feeling dissatisfied.
The article goes on to state that when a healthcare facility is understaffed, the same amount of work falls to fewer nurses who typically end up working longer hours. Doing so with little to no relief can cause a breakdown in mental, emotional, and physical health.
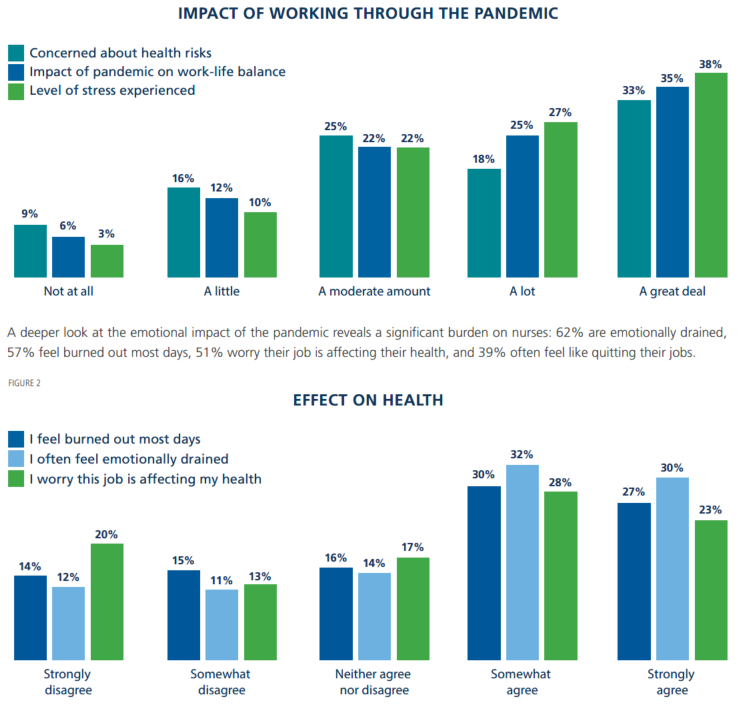
Staffing issues during the pandemic has resulted in this scenario playing out in organizations across the country. Data from the 2021 Survey of Registered Nurses showed that concern among nurses about the impact of the pandemic on their personal and professional lives was high. Sixty-five percent of nurses surveyed answered “a lot” or “a great deal” regarding their level of stress working during the pandemic. Sixty percent responded similarly on how much their work-life balance has been negatively impacted, and 51% had concerns about work-related health risks.
Working in a variable, high stress environment like healthcare is emotionally challenging, and there are physical demands of bedside care that can lead to injuries. On top of that, there are the stressors of most other shift-work professions, e.g., schedule issues, perceived inability to take a vacation, problems with managers and other co-workers, etc. All of this can leave nurses and other providers struggling, often within a few years of beginning their career. Feelings of exhaustion, increased mental distance from one’s job, negative or cynical feelings about the job, and reduced professional efficacy are all symptoms of working in high stress environments.
Healthcare executives are fully aware of the challenge of provider burnout, according to the 2021 Healthcare Trends Survey Report. In fact, they rated it as potentially the most disruptive force hospitals and health systems will face in the next three years.
Positive Change Starts in an Unlikely Spot
While these signs are discouraging, there are reasons for optimism as well. Tangible strategies and solutions can be implemented to reduce this stress, provide managers more time to support their teams, and ensure staffing can be coordinated more efficiently.
One piece of good news from the Healthcare Trends Survey is that engagement among leadership and healthcare professionals is high, despite the challenges of the last 18-plus months. Leaders were deemed highly engaged by 76% and moderately engaged by 21%. For physicians and nurses, 91% and 92% were at least moderately engaged, respectively. A takeaway from this study is that battling COVID-19 has pulled many clinicians together, generating incremental improvement in engagement.
Another encouraging result from the 2021 Survey of Registered Nurses is that through the challenges of the pandemic a large majority of nurses retain a fundamentally positive view of their profession. Over the years, RN surveys by AMN Healthcare have shown persistently high career satisfaction among nurses, and the pandemic has only marginally affected this. Nurses remain very proud to be nurses, provide quality care to patients, teach the next generation, and lead organizations.

With this passion and the incredible resiliency of healthcare professionals as motivation, changes can be made through the process of talent planning. This positive change starts in what some may think is an unlikely place: The finance department.
Every Journey Starts with a Plan
A healthcare organization’s finance department provides productivity targets and staffing matrices for other departments across their system. These are financial instruments that indicate how many and what types of staff are needed at certain demand points. However, it is common that even organizations with strong financial teams are producing targets that do not reflect the reality of the departments providing care. Typically, this is because those who are making daily staffing decisions (charge nurses, house supervisors, staffing offices, patient placement teams, etc.), are not involved in budgeting conversations nor have the proper training to be budget minded, as they typically come from clinical backgrounds.
An important component of talent planning is conducting a staffing plan assessment. This looks at four distinct areas to evaluate accurate staffing levels and identify productivity, financial and operational opportunities.
- Identify appropriate staffing levels for each department
- Understand the staffing needed based upon actual and predicted patient or workload volumes
- Quantify the financial impact of productive plans
- Look for additional cost savings measures and a pattern of exceeding targeted wage rates with unproductive outcomes
Before any talent planning initiative is started, organizations should implement a solution design process. This is a collaborative process that helps health organizations navigate their initiatives. This model compels an organization to truly understand the talent challenges they are trying to solve and creates a framework for a shared vision of what success looks like, as well as the path to get there.
Acquiring the Right Mix of Talent
Once the initial work of a staffing plan assessment is done and targets are set, an organization can assess the gaps in what appropriate staffing levels should be and what talent is already employed within the health system. Keeping recruiting for diversity on track is another factor essential to a healthcare system’s long-term success. From there, the work begins to acquire and develop the full spectrum and sources of talent to deliver great patient care.
When recruiting permanent staff, healthcare organizations can partner with a talent acquisition company to outsource recruitment services or use those services to supplement an internal team. Partnering with a recruitment solutions firm (also referred to as RPO) enables quick and efficient hiring of quality candidates while lowering cost, ensuring a good cultural fit, and providing a better patient experience.
Supplementing permanent staff with contingent staff is where many organizations can get bogged down with all the components, various staffing agencies, and administration. Utilizing a managed services approach allows a workforce solutions provider with specific expertise to bear responsibility for the recruitment and development lifecycle, optimizing core and contingent talent to increase efficiency and reduce costs. Some providers also support key processes such as vendor management, scheduling logistics, and credentialing without the burden falling on talent acquisition teams.
Vendor or staffing agency management, is an area that can be simplified with a vendor management solution. Vendor management solutions (VMS) are centralized, vendor-neutral portals enabling healthcare facilities to quickly staff and manage their contingent talent. Some solutions utilize a bid-driven marketplace, ensuring fair market rates. Deployment of a VMS eliminates time-consuming phone calls and emails to various supplies while greatly increasing the candidate pool.
Proactively Managing Talent to Deliver Care
Having the needed talent in place is an important and necessary step, but the next area of focus, proactive management of scheduling and staffing, can make all the difference in the drive to support healthcare professional well-being and improve patient outcomes.
The first focus is to examine staffing and scheduling policies and how they are being applied across the organization. Staffing practices should be analyzed on the unit and department level and then streamlined wherever possible across the entire hospital or health system for consistency. Adopting this enterprise mentality will create better transparency about staffing needs and opens the door to sharing resources through centralization. It also promotes fairness and increases morale because staff know the playing field is equal and all are working under the same set of policies and expectations.
The promotion of fairness and morale-boosting strategies can be carried over to how schedules are developed. There are several strategies that provide healthcare professionals input and choice in the creation of schedules. Self-scheduling has long been a popular method among nurses. With the right framework, self-scheduling can augment more traditional scheduling methods, providing more work-life balance for caregivers. Additionally, open shift management tools can allow staff to select shifts where there are needs. The shifts of greatest need can be incentivized weeks in advance, providing a win-win for the organization and the healthcare professional.
Centralization is a key element of the efficient deployment of staff the day of the shift. Utilizing a scheduling tool that provides the ability to see staffing across an entire health system, centralized staffing offices can view staffing levels and needs, allowing more strategic placement of healthcare professionals to smooth staffing across the system.
Conclusion
In a field where compassion is at the heart of “the mission,” it is reasonable to expect that compassion can be the leading edge of improving the patient experience.
Compassion for healthcare professionals and the implementation of talent strategies and solutions that keep their wellbeing at the forefront will allow them to be at their best every day. When healthcare professionals are better supported, patients receive better care, enabling them to live their healthiest possible life.
For more information on how we can partner to use talent planning strategies to improve caregiver well-being and the patient experience at your organization, visit AMNHealthcare.com/MSP or contact client services@amnhealthcare.com.