Hospitals today face compressed reimbursements and strict Medicare and Medicaid payment requirements. To ensure success amid these circumstances, providers are striving to optimize patient flow and reduce the length of stay. However, achieving these goals is no easy feat.
Healthcare operations are complex. The volume and acuity of patients is highly variable. Care delivery requires complex coordination of people and processes. And frontline teams have data overload that doesn’t support on-the-fly decision-making.
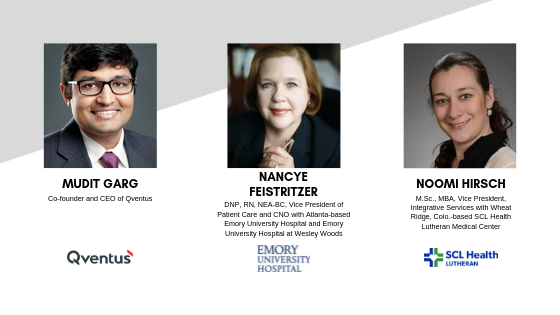
At Becker's Hospital Review's 10th Annual Meeting in Chicago, Scott Becker moderated a panel about improving patient flow with the application of predictive analytics and intelligent automation. Panelists included:
- Nancye Feistritzer, DNP, RN, NEA-BC, Vice President of Patient Care and CNO with Atlanta-based Emory University Hospital and Emory University Hospital at Wesley Woods
- Noomi Hirsch, M.Sc., MBA, Vice President, Integrative Services with Wheat Ridge, Colo.-based SCL Health Lutheran Medical Center
- Mudit Garg, Co-founder and CEO of Qventus
During the discussion, panelists outlined how people, processes and technology can be collectively leveraged to improve communications, eliminate bottlenecks and decrease the length of stay.
Patient flow 1.0: Leveraging people and processes
When Dr. Feistritzer arrived at Emory University Hospital in 2014, she helped launch a comprehensive initiative to improve patient flow. The initiative included the creation of a patient flow center focused on data analytics, a steering committee with C-level members and a lean operating model to engage frontline employees. Despite these efforts, the organization still lacked real-time access to data.
Around six years ago, SCL Health Lutheran Medical Center in Wheat Ridge, Colo., experienced an increase in negative patient comments about its discharge process. Like Emory University Hospital, the organization also focused initially on people and processes to address patient flow.
"We completed a lean analysis of our discharge process," Ms. Hirsch recounted. "From the time a physician entered a discharge order to the time the patient was wheeled out, there were 279 steps and only one-third of those were value-added to the patient."
Lutheran Medical Center analyzed its processes one by one to reduce length of stay and streamline its discharge process. After addressing the low-hanging fruit, however, the organization hit a plateau.
To reduce length of stay further, both Emory University Hospital and Lutheran Medical Center recognized they needed technology that supported a system of action for patient flow.
Patient flow 2.0: Utilizing a system of action
A system of action focuses on three capabilities:
- Proactive identification of issues based on real-time data
- Seamless orchestration of actions for frontline teams
- Continuous management of high performance and reinforcement of desirable behaviors
To take patient flow to the next level, Lutheran Medical Center and Emory University Hospital implemented the Qventus system of action, a technology platform powered by artificial intelligence and machine learning that optimizes patient flow.
Lutheran Medical Center hoped to streamline discharge planning in its two most challenging units: medical and surgical. "Qventus organizes information so that discussion points surface automatically during rounding. It also measures quality, such as the accuracy of the estimated discharge date and how often clinicians enter that date into the system," Mr. Garg said. As a result, discharge planning conversations are more structured.
"We've seen a major leap in physicians entering an estimated discharge date into Qventus. It went from less than five percent to the high 80s. This underscores the buy-in and partnership we have with physician groups," Ms. Hirsch said. Qventus has also improved the internal communication flows. Care managers now save 30 to 60 minutes daily when communicating patient information within their own team. The two units where the solution was first launched have documented 0.3 and 0.5 days reductions in length of stay.
Emory University Hospital has also seen 0.7 days reduction in length of stay where the Qventus system has been implemented across eight medicine units.
"Physicians, nurses, social workers and rehab therapists now partner as a team. Qventus has given them a new line of sight into flow issues," Dr. Feistritzer said.
Qventus has generated a 23 percent reduction in length of stay in Emory University Hospital's post-anesthesia care unit. "The system uses nudges to identify bottlenecks and ensure coordination," explained Mr. Garg.
Conclusion
Optimizing patient flow with a system of action starts with great leadership and operationalization of technologies. In addition to hospital-specific improvements, institutions can use a system of action across an entire hospital system to transfer and load balance resources across different facilities. "At the end of the day, the mix of people, process and technology is where the magic happens," Mr. Garg observed.
For more information, please visit www.qventus.com or email info@qventus.com.


