A new model for improving hospital care
The following content is sponsored by TeamHealth.
Hospitals across the country are looking for innovative ways to improve the delivery of healthcare to lower costs, increase patient satisfaction and enhance patient outcomes. With mounting evidence that the patient-centered medical home model is effective on all of these fronts, hospitals should consider applying the principles of this primary care model to the inpatient hospital setting in a new model for care: the patient-centered hospital home.
Understanding medical homes
To understand the patient-centered hospital home, one must first understand the patient-centered medical home. According to a 2007 report authored by several national physician organizations, the PCMH is defined as "an approach to providing comprehensive primary care for children, youth and adults. The PCMH is a healthcare setting that facilitates partnerships between individual patients and their personal physicians, and when appropriate, the patient's family."
The goal of a PCMH is to improve healthcare by transforming the way primary care is organized and delivered. Providing primary care that prevents illnesses and recognizes and treats health problems early can improve health outcomes, help patients better manage chronic diseases and lower costs for patients, providers and payers.
In recent years, the PCMH has gained widespread favor. Provisions of the 2010 Patient Protection and Affordable Care Act included strategies for enhancing primary care and medical homes. According to the National Academy for State Health Policy, 43 states had adopted policies and programs to advance medical homes as of April 2013.
And many PCMHs are delivering results. For example, BlueCross BlueShield of Michigan's PCMH saved an estimated $155 million over its first three years. In Boston, a PCMH serving seniors increased rates of immunization, mammography, colorectal cancer screenings and eye exams. And a 2012 review of 46 medical home initiatives nationwide concluded that the "PCMH improves health outcomes, enhances the patient and provider experience of care, and reduces expensive, unnecessary hospital and emergency department utilization."
Defining the patient-centered hospital home
Unfortunately, the PCMH does not impact the way care is delivered in the inpatient setting. That's why the patient-centered hospital home is so important.
The PCHH is an approach to providing highly effective, coordinated care to patients during a hospital stay. The PCHH is a hospital-based care setting that provides a physician-led, multidisciplinary and team-based system of patient-centered care that guides the patient throughout the entire hospital experience, from initial diagnosis and admission through discharge and beyond.
To put it simply, the PCHH applies the functions and attributes of the PCMH model to the inpatient setting, with the goal of making the entire continuum of hospital-based care safer, more efficient and effective — as evidenced by better patient outcomes and satisfaction and lower costs.
PCHH: Why now?
Accountable payment models and value-based purchasing require highly coordinated, integrated care — something many hospitals struggle to achieve. Most hospitals function in a fragmented manner with different departments operating in self-contained "siloes." Rife with inefficiencies, miscommunications and delays, this operating model can be costly both in terms of actual dollars and patient outcomes.
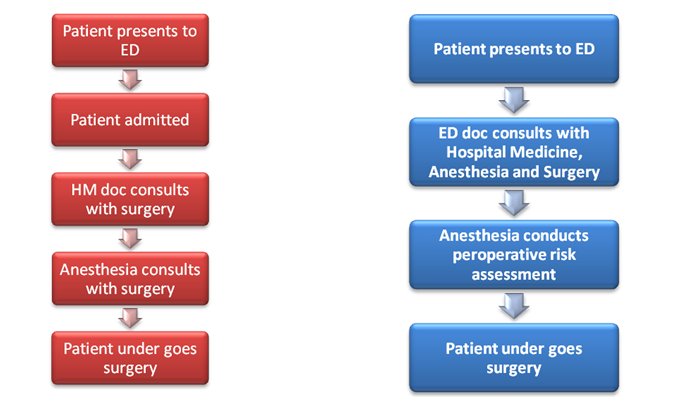
For example, in a typical hospital, the process of caring for an elderly patient with a hip fracture goes something like this:
The patient receives an X-ray and pain medication in the emergency department. Once the ED physician diagnoses the hip fracture, he or she hands off the patient to a hospitalist who admits the patient, conducts an assessment and requests a consultation with a surgeon. It may be several hours before the surgeon is able to see the patient, obtain clearance for the surgery and consult with the anesthesia department to make sure the patient is surgery-ready. At that point, the anesthesiologist may need to run additional tests prior to surgery.
In this scenario, it may be 36 hours before the pre-surgical process begins. In fact, many hip fracture patients face a costly three-to-five-day inpatient wait for surgery. In 2011, the mean cost for a hospital stay for a hip fracture was $15,400, according to the Healthcare Cost and Utilization Project. And for high-risk, older patients, longer hospital stays increase the chances of infection, complications or even mortality. According to the Centers for Disease Control and Prevention, one out of five hip fracture patients dies within a year of their injury.
PCHH solution
If, however, the hospital adopts a PCHH approach to care, it can implement more efficient protocols and pathways for managing high-risk, high-cost cases with greater focus on the entire inpatient continuum.
In a PCHH model, after the ED physician confirms a hip fracture, he or she immediately notifies the anesthesia and hospital medicine teams. The hospitalist admits the patient using more standardized order sets, and the anesthesiologist notifies the orthopedic surgeon, schedules the surgery and does a pre-operative risk assessment before the patient heads to surgery. In many cases, the patient can receive surgery the very same day.
This rapid hip protocol improves communication among providers and creates a streamlined patient experience. The model has been shown to dramatically lower length-of-stay, reduce the likelihood the patient will need a blood transfusion, and lessen the risk of post-operative infection, consequently cutting the patient’s rehabilitation time. These improvements not only save the hospital time, money and bed capacity, they help ensure better outcomes.

Benefits of PCHH
In general, when the PCHH approach is successfully applied to hospital-based care, benefits can include:
• Preventing unnecessary or repetitive testing
• Avoiding unanticipated ICU admissions
• Preventing cancelled/delayed surgery
• Reducing length of stay
• Improving patient satisfaction
• Managing and facilitating the transition of care at discharge
• Preventing unnecessary readmissions
• Decreasing the need for blood transfusion
• Decreasing risks from post-operative infection
Building the PCHH
To create an environment where all departments work together, hospitals must integrate service lines. Departments must be willing to communicate with one another to treat patients in a way that considers the patient's entire hospital experience and potential outcomes, not just the treatment delivered by the individual provider at a fixed point in time.
Hospitals should convene the most important participants in the PCHH to build consensus around this new approach to delivering care, including the following departments:
• Emergency medicine
• Hospital medicine
• Anesthesiology
• Surgery
Once all team members understand their roles, hospitals should begin looking at the specific diagnoses where they can best collaborate to produce better outcomes for the patient and hospital.
Surgery and anesthesia
In most hospitals, somewhere between 70 percent and 90 percent of all patients will need some sort of procedure or surgery during their stay, and approximately 65 percent to 70 percent of the costs of inpatient care come from surgical or procedural practices. The importance of surgical services makes it a natural place to begin a new focus on a coordinated, integrated, inpatient care model.
In fact, the American Society of Anesthesiologists is developing the Perioperative Surgical Home model as a way to provide better coordinated care throughout a surgical patient's stay. In the Perioperative Surgical Home, patients who need surgery are managed by a coordinated, multi-disciplinary team from pre-operative assessment through the post-discharge period with the goal of reducing issues such as duplicate testing, surgical complications, and lengthy hospital stays while providing safer, more cost effective care.
For hospitals looking to become a patient-centered hospital home, the perioperative surgical home provides a strong base for expanding a coordinated model of care throughout the inpatient setting.
Challenges and opportunities
Re-engineering care protocols for a PCHH model can be a challenging process. Because physicians coming together under a PCHH are used to working independently, garnering the necessary buy-in and achieving practice pattern changes may be very difficult. This is particularly true if all the participating departments are operated by independent physician groups that have no incentive to work together, stay later or undertake whatever additional tasks may be required under new care models.
One way to overcome this challenge is through consolidated service lines. Hospitals that choose to partner with a clinical outsourcing provider with the resources and experience in integrated care "home" models can, for example, create shared incentives for providers to work together on new care protocols. Together, the hospital and clinical partner create a shared-risk pool based upon mutually desirable metrics that are tied to quality and service outcomes. If the provider teams achieve those metrics, then all involved physicians would benefit from the shared savings. This approach helps ensure that all providers are sufficiently motivated to do their part, even if it requires additional effort, so hospitals and patients can reap the rewards of better patient outcomes and lowered costs.
Conclusion
Transformations in the healthcare industry linking payments to quality are requiring hospitals to develop new approaches to delivering care to operate more efficiently, improve outcomes and achieve high levels of patient satisfaction. By adopting the PCHH approach to care, hospitals can break down the internal siloes that cause costly inefficiencies, providing care in a multidisciplinary, coordinated way that allows for better health outcomes for patients and better financial outcomes for the hospital.


