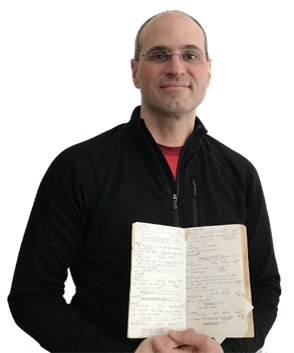
Not so long ago, physician charts were much simpler. For example, in the photo below my husband is holding his entire pediatric medical record:
Editor's Note: This article originally appeared on December 5th, 2017 on Allscripts Blog: It Takes a Community
Today’s physicians, however, are overwhelmed with documentation burdens. According to a study published in the Annals of Internal Medicine, physicians spend more than half of their time on electronic health record (EHR) and other desk work.
Doctors have always taken notes, so why is it so much worse today? These notes are for more audiences than ever before. And, while it adds a richness to the data, we should not overlook a significant hidden cost: physician burnout.

Evolution of physician record keeping
As the medical community kept adding audiences for physician notes, they kept getting longer and longer. Let’s use an example of documenting a visit with a three-year-old patient with an ear infection, who is otherwise healthy:
Just for me – In the earliest days, doctors kept notes only to remind themselves. They could use their own shorthand to document an ear infection and would indicate the date, Otitis Media (ear infection) in the right ear and prescription. The note could be short and sweet: 6/7/17, Right OM, Amox.
+ my team – Personal note taking doesn’t always provide enough context for other members of clinical teams, whether it be a follow-up visit with a partner on call or nurse responding to questions over the phone. The note gets a bit longer: 6/7/17, symptoms for 3 days w/fever on day 3, Right OM, Amox for 10 days.
+ attorneys and payers – To reduce risk for legal liability and meet insurance company requirements, the physician’s note must also capture patient history, physical exam points, subjective assessment and a documented follow-up plan.
Now the note looks more like this: 6/7/17, Subjective: Patient presents with 3 days runny nose, cough and awakened last night with fever and right ear pain. Last ear infection was 11/25/16. No vomiting, diarrhea, rashes. Patient is drinking well, but eating less than normal.
Objective:
- Vital signs: temp 101, HR 98, RR 20
- General: Cranky, but alert without respiratory distress
- HEENT: eyes without redness or discharge, nose with clear rhinorrhea, pharynx with mild erythema, left TM normal, right TM red and bulging
- Lungs: clear to auscultation bilaterally
- Heart: regular rate and rhythm without murmurs
- Abdomen: soft and nontender
- Skin: no rashes, good turgor
Assessment: URI complicated by right otitis media which is currently well-tolerated.
Plan: Supportive care reviewed. Amoxicillin as prescribed. Recheck if symptoms worsen or persist.
+ ICD-10 – Physicians have not traditionally had depth of expertise when it comes to billing codes, and now with ICD-10, there are 38 separate codes for ear infections. Which one should we add to the note above?
- H66.001 Acute suppurative otitis media without spontaneous rupture of ear drum, right ear
- H66.004 Acute suppurative otitis media without spontaneous rupture of ear drum, recurrent, right ear
- H66.41 Acute suppurative otitis media, right ear
- H66.91 Acute otitis media, right ear
+ government – Incentive programs, such as Meaningful Use, add another layer of expectations for physician notes. This can mean wider responsibility for healthcare services that may not be relevant during the visit, requiring pediatricians to record blood pressure readings for toddlers complaining of ear infections, podiatrists to ask about flu shots and orthopedic surgeons to make sure every woman over 40 has a mammogram.
+ patients – I enthusiastically support patients having access to their own records. If it helps patients understand and take control of their health, it is a very good thing. However, it adds more complexity to physician notetaking. For example, “right OM” or even “right otitis media” is not as immediately recognizable as “ear infection, right ear.” Physicians must write comprehensive, clear notes, without causing unnecessary worry.
Relieving documentation burden and burnout
These audiences all need slightly different things from notes, and they all have a role to play in helping the industry reduce costs and improve outcomes. Physicians continue to have a central role, and here are four ways they can proactively manage documentation expectations:
- Explore data entry options with the EHR. Does it have to be clicks or typing or can it be voice recognition? Are there shortcuts you can use for most commonly used orders, codes, and communications?
- Determine if there is administrative work that can be delegated to support staff.
- Find out if there are new features of the EHR that may not have been available or selected when first implemented.
- Be active in the process. Participate in the organization’s efforts to improve.
Some organizations are using health IT in creative ways to relieve the pressure. Some address the process by using scribes or voice recognition software, others are vigilant about frequently optimizing workflows for maximum efficiency.
Most organizations recognize that physicians should not bear the entire responsibility for documentation and are seeking ideas and solutions that will improve physician, and by extension, patient satisfaction. It’s time for the industry to take more steps to improve provider wellness by reducing the burdens of health IT.
Learn more about how Allscripts helps improve the clinician experience.


