Changing payment systems are putting pressure on hospitals to deliver value. Value is defined as quality, for a reasonable price. As hospitals and health systems strive to decrease the costs of the delivery of care while simultaneously increasing the quality and patient experience, multiple alignment strategies are being explored.
Co-management and bundled payment two strategies hospitals are using to align with physicians to improve quality and lower costs.
Co-management is a quality-focused approach where the hospital and physicians partner to "co-manage" a defined set of services. The hospital pays the physicians to co-manage the patient experience in quality, efficiency and experience. The scope of the management services are jointly defined by diagnostic related group and outpatient procedures.
The legal arrangement may take the form of a new company or an all-party agreement that defines structure and the scope of responsibilities. This structure meets all federal, state, Stark Law and anti-kickback regulations. A fair market valuation is completed on the size and scope of the service line to set the management fee.
Physicians who are regularly present at that hospital are invited to join in the co-management process. Payment is in the form of a fixed fee, an hourly rate to cover their monthly work activity. A variable fee is available as an incentive, if agreed upon goals are met. The agreement is then revisited each year, in terms of scope, participating physicians and goals for the year.
It is important to setup the co-management arrangement to fit clearly within the Stark and anti-kickback safe harbors. In December 2012, the HHS Office of Inspector General issued Advisory Opinion No. 12-22, related to a cardiovascular co-management agreement and found it to be appropriate. In that particular agreement, the group was paid a fixed and incentive fee. The opinion serves as a good reference outlining the steps to follow in order to fit within the safe harbors as defined by 42 CFR 1001.952 d.
The government's effort to move to bundled payments has a long history. In 1990, CMS initiated the Medicare Coronary Artery Bypass Surgery pilot project with four hospitals. This project included the inpatient stay and physicians treating these patients. Results of this project remain significant.
In January 2012, the Congressional Budget Office released a report reviewing the outcomes of Medicare's value-based purchasing models. The Medicare Coronary Artery Bypass demonstrated economic savings to Medicare of 10 percent, but the report stated that other demonstrations of value-based payment appear to have produced little or no savings for Medicare. The most recent implemented bundled payment project by Medicare is the acute-care episode demonstration project launched in four states in January 2010. Additionally, in August 2011, CMS announced new projects as part of its Bundled Payments for Care Improvement initiative. The project participants awarded are slated to begin bundled payment in the summer of 2013.
The idea behind bundled payment is to align physician and hospital incentives in the care of the patient. Hospitals are responsible for the cost of care but it is physicians who control the majority of these costs. The physicians determine what products and services to use and the length of the hospitalization. The new models involve the hospital taking a discount to the current payment for the facility side, and allow the hospital to share any savings back with physicians. Physicians have the opportunity to earn up to an additional 50 percent of their total professional fees on the care of that patient, based on improvements in cost, quality and patient care. This economic alignment that pays for cost efficiency and quality is known as gainsharing. Gainsharing programs that achieved approval from the OIG demonstrated the value of hospital-physician economic alignment in controlling costs while maintain quality.
This joint effort has been proven to be effective at aligning physicians with the hospital, but also with other physicians in that specialty. With all physicians who are active at the hospital invited to join, ideas are shared, protocols are discussed and processes refined. Physicians are put onto teams that have specific goals in the program. Suddenly, they have discussions on quality of care. The variations narrow, and efficiencies improve.
Bundled payment initiatives build on these same concepts but require an additional level of commitment and trust between the physicians and hospital.
Co-management agreements work when they bridge that chasm, creating an opportunity to see the other view and to work together. For this reason, they are a good stepping stone toward bundled payment relationships. If there is not yet a level of baseline trust, dividing the payments can be a very tricky road to navigate.
Bundled payment measurements move co-management from a service-line focus to an individual physician performance on a per patient basis. In a bundled payment, an individual physician can earn a gainsharing payment by meeting quality targets and lower costs without participation from all physicians in a designated specialty. However, in published studies of bundled payments and stand-alone gainsharing programs, there has been significant participation from the majority of physicians participating in these arrangements.
The implementation of bundled payments requires physicians remove variation and work with interdisciplinary teams to achieve high value. Many of the elements desired are designed in co-management agreements. In practice today, we see both coexist. Based on our interactions with hospitals nationally, the identification of the Bundled Payment pilots on Models 1-4 has not impacted the number of co-management agreements we see nationally. They do not at this stage appear to be mutually exclusive but complimentary strategies.
Joane Goodroe is an independent consultant who is responsible for the development of the first gainsharing models approved by the OIG. She has worked with bundled payments since 1990. She continues to consult with hospitals and physicians on new models of care and integration. Contact her at jgoodroe@jgoodroe.com
Gail Peace is president and CEO of Ludi, Inc., a company that helps hospitals and health systems automate, track and actively manage physician-hospital agreements. Ms. Peace has 20 years of healthcare experience developing new partnership structures with physicians and hospitals. Contact her at gail@ludiinc.com.
4 Key Considerations for Transitioning to Bundled Payments
Co-management and bundled payment two strategies hospitals are using to align with physicians to improve quality and lower costs.
I. Co-management defined
Co-management is a quality-focused approach where the hospital and physicians partner to "co-manage" a defined set of services. The hospital pays the physicians to co-manage the patient experience in quality, efficiency and experience. The scope of the management services are jointly defined by diagnostic related group and outpatient procedures.The legal arrangement may take the form of a new company or an all-party agreement that defines structure and the scope of responsibilities. This structure meets all federal, state, Stark Law and anti-kickback regulations. A fair market valuation is completed on the size and scope of the service line to set the management fee.
Physicians who are regularly present at that hospital are invited to join in the co-management process. Payment is in the form of a fixed fee, an hourly rate to cover their monthly work activity. A variable fee is available as an incentive, if agreed upon goals are met. The agreement is then revisited each year, in terms of scope, participating physicians and goals for the year.
It is important to setup the co-management arrangement to fit clearly within the Stark and anti-kickback safe harbors. In December 2012, the HHS Office of Inspector General issued Advisory Opinion No. 12-22, related to a cardiovascular co-management agreement and found it to be appropriate. In that particular agreement, the group was paid a fixed and incentive fee. The opinion serves as a good reference outlining the steps to follow in order to fit within the safe harbors as defined by 42 CFR 1001.952 d.
II. Bundled payment defined
As the national discussion on reform continues, there are many uncertainties with how healthcare will be accessed and paid for in the future. Bundled payments have emerged as a payment mechanism within the Medicare program and with private payors. For this discussion, Medicare's bundled payment efforts will be used to demonstrate concepts. For more than twenty-five years, there have been efforts to combine hospital and physician payments into one bundled fee based on an inpatient diagnosis.The government's effort to move to bundled payments has a long history. In 1990, CMS initiated the Medicare Coronary Artery Bypass Surgery pilot project with four hospitals. This project included the inpatient stay and physicians treating these patients. Results of this project remain significant.
In January 2012, the Congressional Budget Office released a report reviewing the outcomes of Medicare's value-based purchasing models. The Medicare Coronary Artery Bypass demonstrated economic savings to Medicare of 10 percent, but the report stated that other demonstrations of value-based payment appear to have produced little or no savings for Medicare. The most recent implemented bundled payment project by Medicare is the acute-care episode demonstration project launched in four states in January 2010. Additionally, in August 2011, CMS announced new projects as part of its Bundled Payments for Care Improvement initiative. The project participants awarded are slated to begin bundled payment in the summer of 2013.
The idea behind bundled payment is to align physician and hospital incentives in the care of the patient. Hospitals are responsible for the cost of care but it is physicians who control the majority of these costs. The physicians determine what products and services to use and the length of the hospitalization. The new models involve the hospital taking a discount to the current payment for the facility side, and allow the hospital to share any savings back with physicians. Physicians have the opportunity to earn up to an additional 50 percent of their total professional fees on the care of that patient, based on improvements in cost, quality and patient care. This economic alignment that pays for cost efficiency and quality is known as gainsharing. Gainsharing programs that achieved approval from the OIG demonstrated the value of hospital-physician economic alignment in controlling costs while maintain quality.
III. The differences in co-management and bundled payment
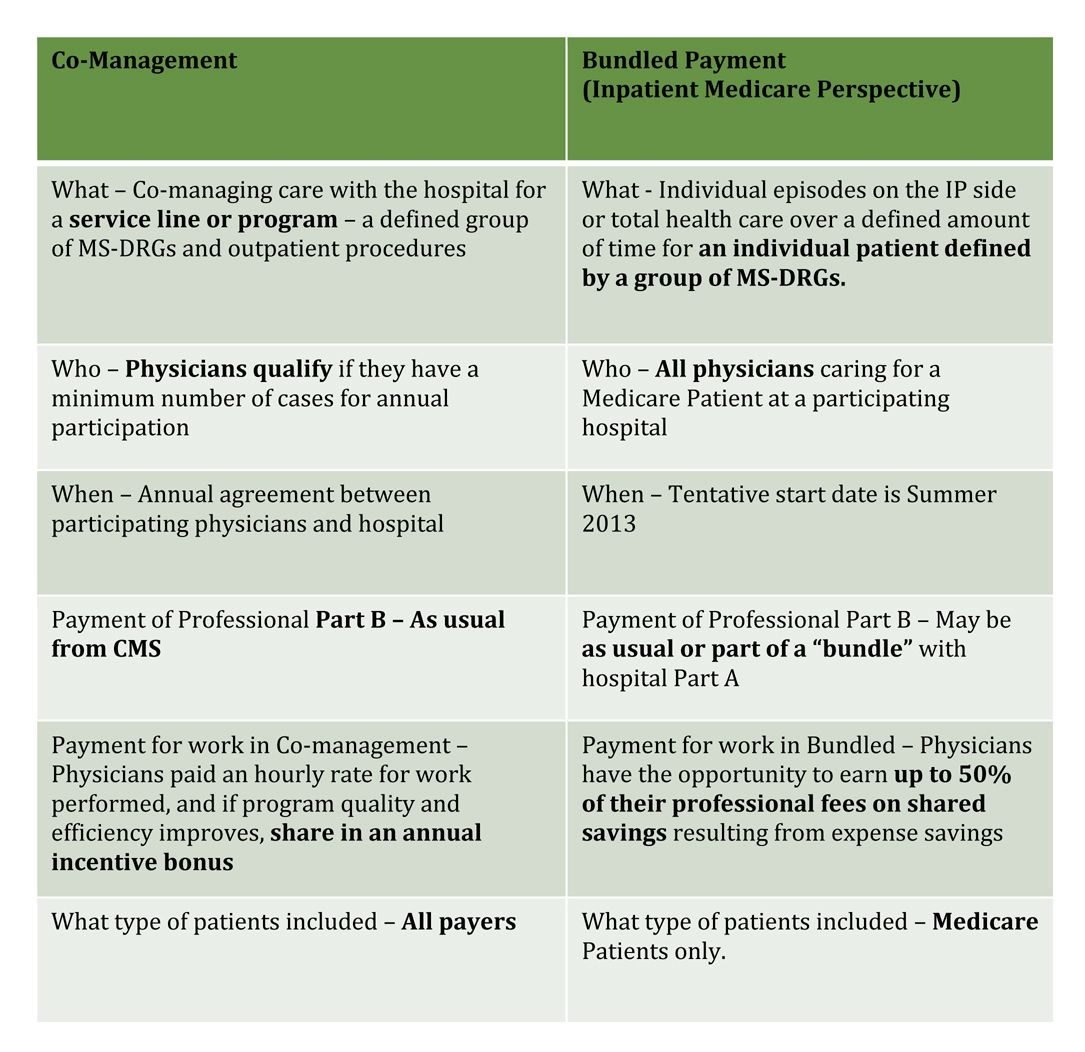
A comparison chart illustrates the differences between co-management and bundled payment. At a high level, co-management refers to a program where physicians qualify to participate in an annual fixed fee for time spent and an incentive bonus that is funded by the hospital. On the other hand, bundled payment is a program focused on individual physician performance on individual Medicare patients from both a quality of care and utilization of resources. The chart addresses the inpatient portion of bundled patients only.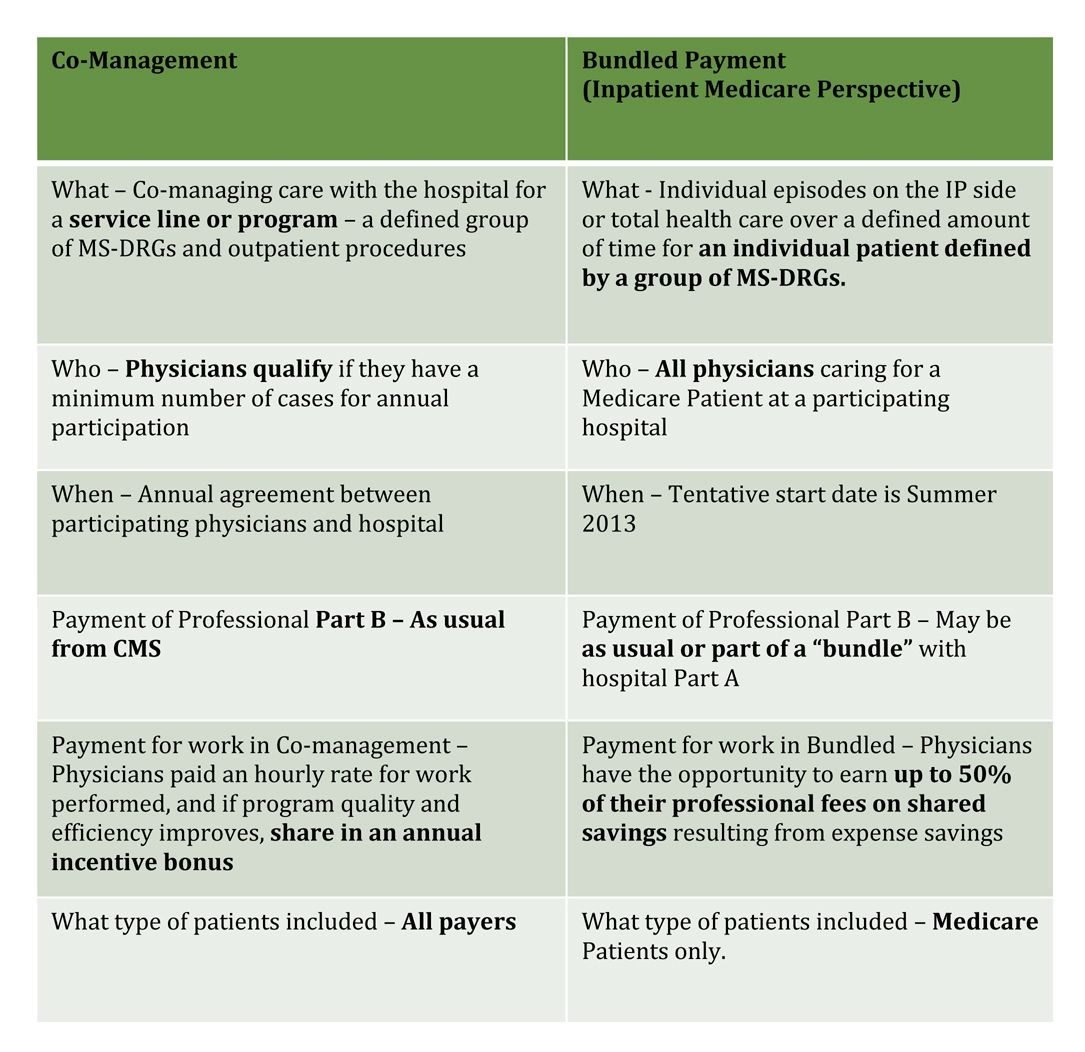
IV. Expected outcomes
Co-management is a physician alignment strategy that puts physicians at the table together with the hospital. If managed appropriately, the physicians make a shift from considering the hospital a separate entity to thinking of the program as their own. The incentives run annually and on program performance, so they also focus on the group and how to move the bar globally. Physicians see the hospital's view, and vice versa. Physicians are called upon to make recommendations in business decisions, such as staffing, marketing and purchasing decisions. For many, it is their first view of the realities facing hospital administrative teams with respect to budgets and performance expectations.This joint effort has been proven to be effective at aligning physicians with the hospital, but also with other physicians in that specialty. With all physicians who are active at the hospital invited to join, ideas are shared, protocols are discussed and processes refined. Physicians are put onto teams that have specific goals in the program. Suddenly, they have discussions on quality of care. The variations narrow, and efficiencies improve.
Bundled payment initiatives build on these same concepts but require an additional level of commitment and trust between the physicians and hospital.
Co-management agreements work when they bridge that chasm, creating an opportunity to see the other view and to work together. For this reason, they are a good stepping stone toward bundled payment relationships. If there is not yet a level of baseline trust, dividing the payments can be a very tricky road to navigate.
Bundled payment measurements move co-management from a service-line focus to an individual physician performance on a per patient basis. In a bundled payment, an individual physician can earn a gainsharing payment by meeting quality targets and lower costs without participation from all physicians in a designated specialty. However, in published studies of bundled payments and stand-alone gainsharing programs, there has been significant participation from the majority of physicians participating in these arrangements.
V. Mutually exclusive?
Although co-management and bundled payments are two distinct strategies, components of each model are exactly the same. Some in the industry speculate that co-management structures will disappear with the surge of bundled payment programs. Our hypothesis at the start of researching this paper was that bundled payment would replace co-management as an organizational strategy. We also believed that moving forward, those hospitals considering bundled payment not yet involved in co-management would skip this step.The implementation of bundled payments requires physicians remove variation and work with interdisciplinary teams to achieve high value. Many of the elements desired are designed in co-management agreements. In practice today, we see both coexist. Based on our interactions with hospitals nationally, the identification of the Bundled Payment pilots on Models 1-4 has not impacted the number of co-management agreements we see nationally. They do not at this stage appear to be mutually exclusive but complimentary strategies.
VI. Summary
As long as the incentive portion of the co-management agreement rewards different measures than the bundled payment program, both can exist from a regulatory perspective. Both strategies require the hospital to "share" or "invest" in the effort in some fashion, so long term, the hospital may not be able to afford both. At early stage of adoption of bundled payment, it seems both can coexist and return greater than the investment. We believe over time, one model may be sufficient to achieve the clinical outcomes and goals desired. Which model may in fact depend on market dynamics and organization's strategy. In sum, we believe these strategies will co-exist for the immediate future, and are not yet mutually exclusive. Over time, there may be a clear winner, but it is too early to predict. It is more likely both will remain important strategies based on market dynamics.Joane Goodroe is an independent consultant who is responsible for the development of the first gainsharing models approved by the OIG. She has worked with bundled payments since 1990. She continues to consult with hospitals and physicians on new models of care and integration. Contact her at jgoodroe@jgoodroe.com
Gail Peace is president and CEO of Ludi, Inc., a company that helps hospitals and health systems automate, track and actively manage physician-hospital agreements. Ms. Peace has 20 years of healthcare experience developing new partnership structures with physicians and hospitals. Contact her at gail@ludiinc.com.
More Articles on Bundled Payments:
CMS Accepting More Bundled Payment Model 1 Applications4 Key Considerations for Transitioning to Bundled Payments


