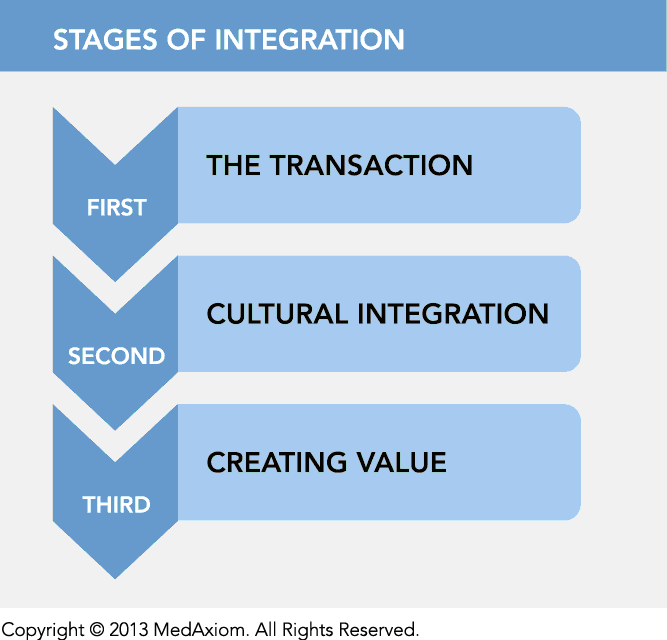
It should not be surprising that the realignment of the industry, merging formerly competing entities, has not been a smooth course. Participants in integration efforts — whether from physician practices or from hospital administrations, experience significant and unanticipated difficulty in effectively merging previously separate organizations. Integrating entities uniformly reported a cadence to the integration process that can be characterized in stages.
Cultural integration is also dominated by the lack of integrated management and data integration. Significant differences in accounting practices, a lack of common language in billing/coding and finance, flexibility and transparency of systems and lack of involvement by department level managers all contribute to often clunky and conflicted initial interactions. Physicians and practice leaders lack of experience in the hospital management structure and approach to problems are often perceived as pushy and beyond scope and authority. These same leaders, accustomed to having management control feel a lack of control and acceptance, are often forgotten in the process. These realities often lead to key leaders feeling diminished, not considered and without the necessary tools to perform their jobs. Pragmatic issues such as fragmented data systems and lack of access to systems and data extending in both directions, coupled with a belief by hospital and practice leaders alike that if only the other would operate as they operate, the organization would be more successful!
Early integrations have taught us that purposeful on-boarding and reorganization of leadership, management and staff roles and responsibilities is not only recommended, but crucial to the new, integrated entity's ability to create value. Successful integrations have taught us that despite the vast differences in the organizations and the people that run them, the multiple perspectives available in each — when combined — is a powerful deployment and capable of delivering the promises for which the integration was initially pursued. Our best learning in cultural integration is knowing that integrating isn't a transaction. Instead, achieving integration takes vision and time to resolve both the physical barriers of system and data integration and, more importantly, the time to resolve the leadership and management barriers therein incorporated.
Suzette Jaskie is president of MedAxiom Consulting and the executive vice-president of MedAxiom. Ms. Jaskie was the CEO of West Michigan Heart and Wisconsin Heart and Vascular in Milwaukee prior to her current position. She also previously served as the executive director of the Frederick Meijer Heart and Vascular Institute, for Spectrum Health System in Grand Rapids, Mich., that governs and manages the cardiovascular service line for the regional health system. Ms. Jaskie has a master's degree in business administration from the University of Hartford and a bachelor's of science degree from the University of Wisconsin.
First stage: The transaction
The first stage of integration is the transaction, and for the last several years — the focus of our efforts. In the transaction stage, typically, the hospital purchases some or all aspects of the practice and enters into either employment agreements or professional service agreements with the physicians. The transaction stage, like all negotiations, require vast (and distracting) attention from all participants, is often conflicted and certainly always emotional. The transaction stage is often long and mismatched in resources available to apply to it — where the hospital typically has many staff and outside consultants, attorneys and valuation firms working on its behalf. The practice usually has the practice administrator and management team, often supplemented by outside legal counsel, but rarely additional resources to supplement the efforts required.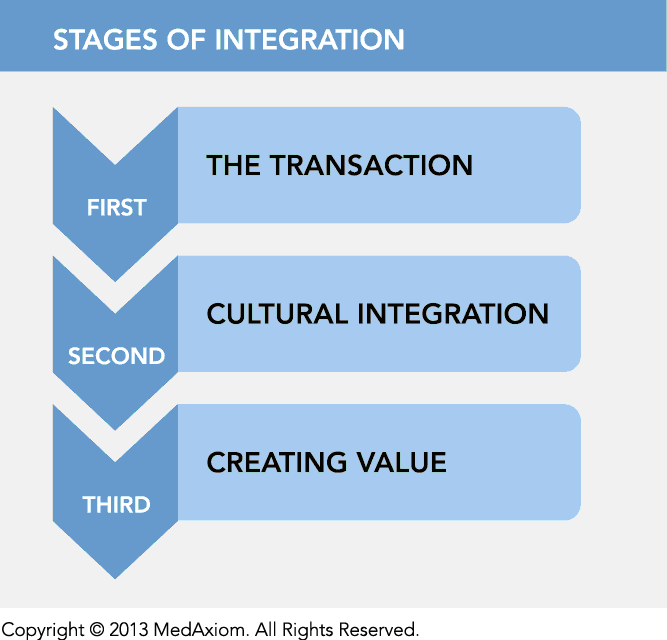
Second stage: Cultural integration
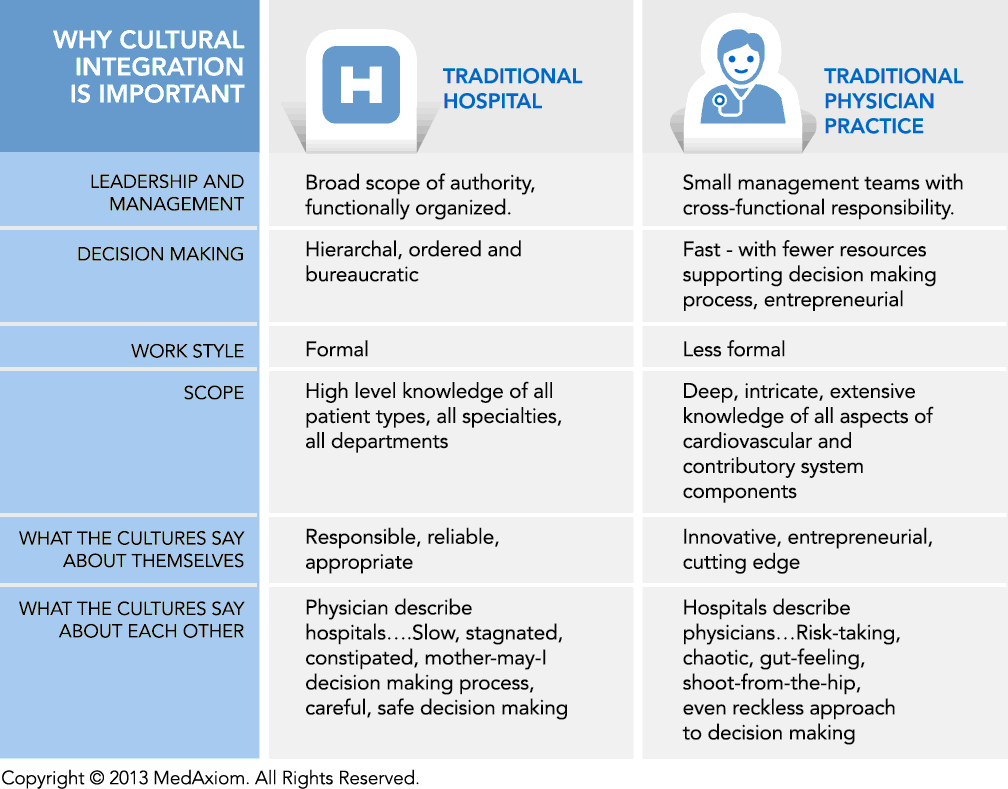
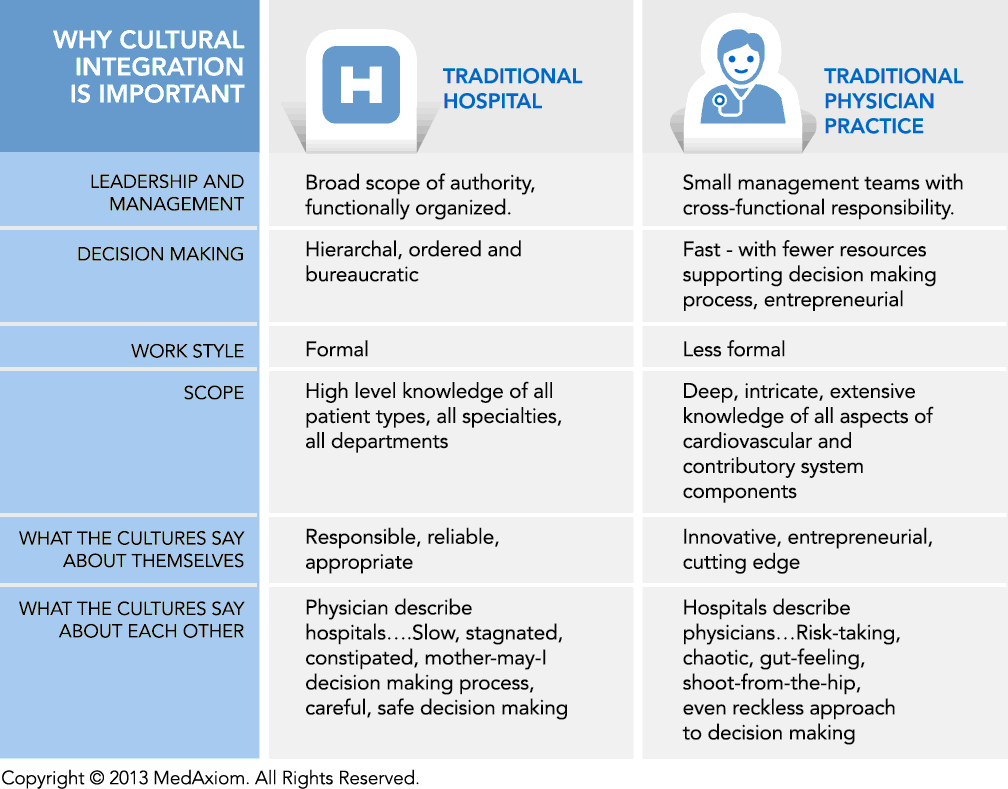
The second stage of integration is, surely, cultural integration. Although there are anecdotal examples of purposeful, well-orchestrated integration of the newly acquired practice into the hospital system and the easy development of shared financial and other data, most practice on-boarding and cultural integration efforts have been less-than-optimally executed. The cultural integration often is two-fold. Not only does the hospital culture and the practice culture need to integrate, but often times cultural integration includes multiple physician groups who additionally must integrate with each other in addition to integrating with the hospital. In cardiovascular, as an example, often multiple cardiovascular specialties (cardiology, cardiothoracic surgery and vascular surgery) and multiple cardiovascular physician groups are simultaneously integrating; many of whom were direct competitors prior to the integration.Cultural integration is also dominated by the lack of integrated management and data integration. Significant differences in accounting practices, a lack of common language in billing/coding and finance, flexibility and transparency of systems and lack of involvement by department level managers all contribute to often clunky and conflicted initial interactions. Physicians and practice leaders lack of experience in the hospital management structure and approach to problems are often perceived as pushy and beyond scope and authority. These same leaders, accustomed to having management control feel a lack of control and acceptance, are often forgotten in the process. These realities often lead to key leaders feeling diminished, not considered and without the necessary tools to perform their jobs. Pragmatic issues such as fragmented data systems and lack of access to systems and data extending in both directions, coupled with a belief by hospital and practice leaders alike that if only the other would operate as they operate, the organization would be more successful!
Early integrations have taught us that purposeful on-boarding and reorganization of leadership, management and staff roles and responsibilities is not only recommended, but crucial to the new, integrated entity's ability to create value. Successful integrations have taught us that despite the vast differences in the organizations and the people that run them, the multiple perspectives available in each — when combined — is a powerful deployment and capable of delivering the promises for which the integration was initially pursued. Our best learning in cultural integration is knowing that integrating isn't a transaction. Instead, achieving integration takes vision and time to resolve both the physical barriers of system and data integration and, more importantly, the time to resolve the leadership and management barriers therein incorporated.
Third stage: Creating value
The third stage of integration is creating value. Only post transaction, given the structure of the integrated relationship and cultural integration, can the hospital and physician organization truly align and perform as an integrated unit. Creating value in the integration is done by empowering the combined governance infrastructure with measured and defined authority, responsibility and accountability to operate, with the charge to improve the quality, operations, financial and market performance of the combined scope of services.Suzette Jaskie is president of MedAxiom Consulting and the executive vice-president of MedAxiom. Ms. Jaskie was the CEO of West Michigan Heart and Wisconsin Heart and Vascular in Milwaukee prior to her current position. She also previously served as the executive director of the Frederick Meijer Heart and Vascular Institute, for Spectrum Health System in Grand Rapids, Mich., that governs and manages the cardiovascular service line for the regional health system. Ms. Jaskie has a master's degree in business administration from the University of Hartford and a bachelor's of science degree from the University of Wisconsin.
More Articles on Integration:
4 Contemporary Issues in Hospital, Physician-Practice Integration
The Cardiovascular Service Line Approach: Creating Value in Organization Structure


