In most healthcare organizations, performance improvement is a process that never ends.
Either driven by the demands of regulators, recognition of risks, or a desire to achieve world-class performance, healthcare executives invest heavily in performance improvement across the enterprise. This takes the form of dedicated improvement teams supported by experts in facilitation and improvement methods. Many hospitals have organized these efforts into formal "project management offices" to coordinate the volume of activity and to ensure projects are completed on a timely basis and with good results.
In any improvement effort, management is inevitably faced with a range of decisions:
- Why improve?
- When to improve?
- How to improve?
- What and where to improve?
"Why and when" to improve is generally driven by a sense of urgency. The focus on readmissions as a result of threatened penalties under the ACA demonstrates this perhaps better than any other improvement opportunity. Within a few months after the ACA was ratified, scores of conferences and related projects focused on reduction of readmissions came into being. "How to improve" is driven by how far the organization wishes to take its improvement capabilities: PDSA/PDCA, Lean and Six Sigma all represent good improvement methods that have a track record for producing good results in all types of organizations, both inside and outside the healthcare industry.
It is "where" to improve that represents the biggest challenge for healthcare organizations. In what Peter Drucker described as "the most complex organization ever devised by man," the choice of where to improve can easily result in analysis paralysis – there are so many opportunities at any given moment. It is not only important to "do things right," cautions Stuart Wesbury, president-emeritus of the American College of Healthcare Executives. You also need to be "doing the right things."
Unfortunately, this is where healthcare organizations face the greatest challenge. It is not uncommon for hospitals to maintain several dozen projects in various stages of execution, with a list of 100+ different improvement opportunities not yet evaluated or initiated. The risk of resourcing projects of marginal benefit is high, particularly when the choice of project may be driven by the passion or influence of various stakeholders in the organization, each with different — perhaps even competing — priorities. Even in a relatively small healthcare organization, it is difficult to establish one single view of all critical improvement needs. This is one reason we see the impact of each "bright shiny object."
"We launched a broad-based improvement initiative and allowed participants to pick projects that interested them, only to find that the resulting outcomes, while positive, made very little impact on our bottom line," recalls Cynthia Blair, Vice President for Organizational Improvement and Strategic Planning at Tallahassee Memorial Hospital. "This made it more difficult for us to sustain enthusiasm around continued investment in the initiative. "
Creative Healthcare has monitored hospital use of project management approaches for nearly 20 years. For many hospitals, this function is managed almost entirely in a variety of Excel spreadsheets. There is a level of simplicity in this approach that is attractive, but static spreadsheets make it difficult to keep information current. Additionally, it is not easy to dynamically sort data in a management meeting when the team is trying to tease the most compelling project opportunities, or the status of existing projects, out of an Excel spreadsheet. In our interviews with hospital managers, they contend Excel is adequate to track a single project, but they lose confidence in the reliability of spreadsheets that attempt to track the status of improvement activity across the enterprise.
For healthcare organizations still entrenched in the use of Excel, the challenge includes not only the desire to coordinate, manage and track activity; there is also no effective way to use Excel to collect, evaluate and compare the hundreds of bona fide improvement ideas that come forth with every passing day. Organizations in this situation are left with an imperfect view of the world around them, and a potential false sense of security.
Recalls Ms. Blair: "What we needed and ultimately found was a technical application that made our efforts quantifiable, trackable, and historical, allowing us to create an institutional memory around our improvement activities."
It was probably inevitable that solutions to the challenge faced by Tallahassee Memorial, and many other health systems, would come in the form of a unifying technical application to bring ideas, projects and ROI into focus, allowing them to reduce the sense of chaos around them. It may be less obvious that the systems we've now been using for years — to manage our personal finances — would evolve to take "portfolio management" to an entirely new level.
This practice is now known as "Project Portfolio Management," or PPM, and whether manual or fully automated, it is helping organizations establish a laser focus on the most promising opportunities for improved performance. Moreover, they support the attainment of the Holy Grail for performance improvement professionals: standard work. Everybody is improving, and improving by leveraging the same tools and approaches. The organization not only completes more projects, but does so faster and with greater returns.
How PPMs Work
- A central repository of ideas created by staff
- Ideas are prioritized on a set of criteria as they enter the system
- Management can view ideas and resource the most compelling opportunities
- Staff are assigned projects and document their work within the system
- The system provides tools and just-in-time training to support standard work
- Robust reports are created in real time and automatically distributed to stakeholders (no administrative time needed for report generation)
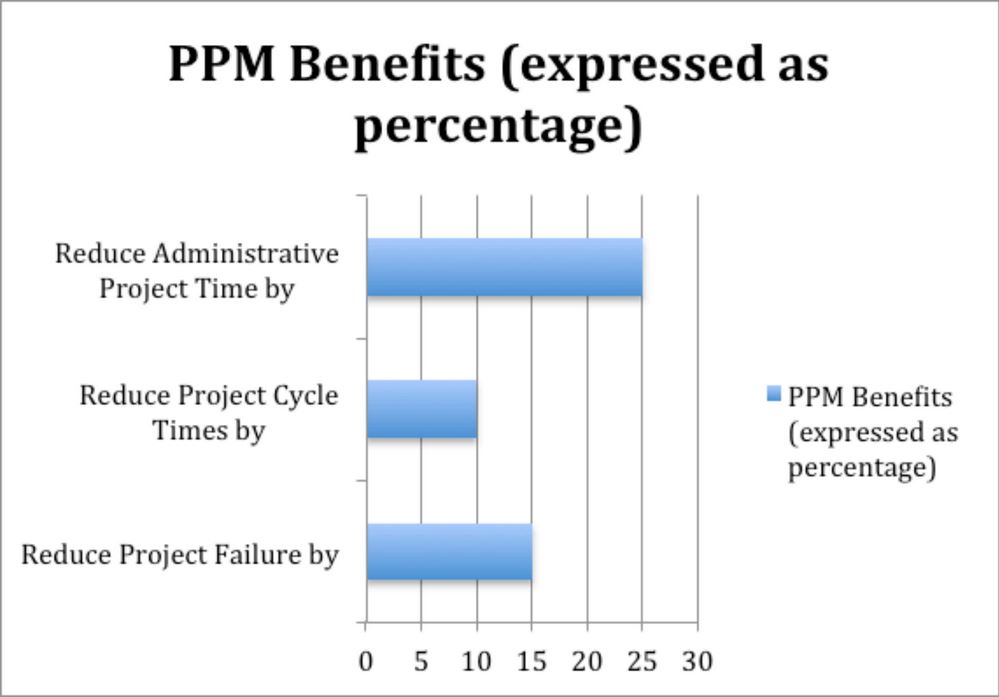
According to PM Solutions Research, a manually-driven PPM approach will deliver returns of 25-50%. Forrester Research finds organizations that utilize an automated PPM can enjoy returns in excess of 250%. (Chart Source: Forrester Research)
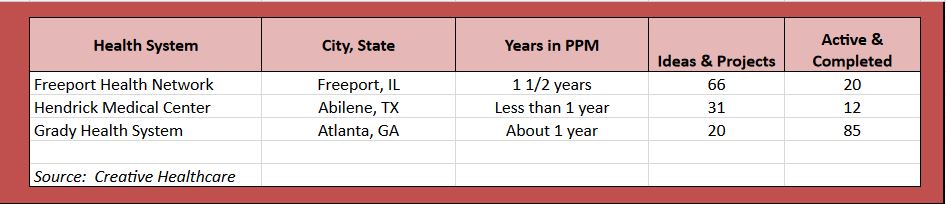
The results predicted by these third-party research organizations is being borne out by specific health systems that have adopted a disciplined approach to portfolio management.
We've profiled below the progression of a few health systems through their adoption of PPM systems and methodologies.
Freeport (Ill.) Health Network
66 Active Projects, 20 Project Ideas
PPM came to FHN just in time. In spring 2014, FHN's executive team, recognizing that the rules of healthcare delivery were changing, issued a challenge: to "transform" the way that care is delivered to its patients.. "In the wake of a changing payer mix, creative disruptions in the market, and other demands of the ACA, 'transformation' became more than a 'nice idea' — it became a necessity," recalls Mark Gridley, COO at FHN.
FHN had a long history of process improvement, so the concept wasn't new to staff — what was new was the magnitude of this challenge. How could FHN completely redesign the way services were delivered? How could they make existing systems smarter, more efficient, less wasteful; enough to improve margins by several million dollars in one year?
FHN's leaders invited staff to source improvement ideas. In the past, they would have likely captured these ideas in some sort of spreadsheet or database; however they launched an automated PPM system, the COMPASS® Quality Management System, at the end of May — and the timing couldn't have been better. Now, directors are able to enter their ideas into one system, providing a detailed business case including estimated financial impact and an assessment of the project's risk and impact. FHN's executive team compares projects at a glance, honing in on those with the highest impact and the lowest risk.
"COMPASS has provided us with a simple, concise means of tracking of our activity." suggests Amy Fisher from FHN. "We now have an 'electronic history book' — we can easily view (and celebrate) every improvement we've implemented in the last year, complete with narratives and metrics."
"Since FHN began its transformation journey in spring 2014, the organization has saved over $2 million through a variety of improvements – reduced waste, standardized products and processes, "right-sized" work, renegotiated contracts, new technologies, and new sources of revenue," notes Amy Fisher, performance improvement coordinator for FHN.. "COMPASS is helping us tell our story," she adds.
Hendrick Medical Center (Abilene, Texas)
31 Project Ideas, 12 Projects Completed in 8 months
Hendrick Medical Center was introduced to the concept of PPM late in 2014, as it began applying Lean concepts to performance improvement and change management initiatives. "As our executive and management staff began Lean training, ideas for future projects begin coming in from all areas — very quickly," recalls Brian Bessent, vice president at Hendrick. "Some project ideas were the 'just do it' kind and some were true process improvement projects that needed Lean principles applied. Either way, we were excited that leaders were beginning to identify areas in our system and were thinking in the right direction."
Like many organizations that launch a change management initiative, Hendrick saw the potential for even more chaos as multiple initiatives were launching at the same time. "We recognized a PPM would allow us to cease the utilization of multiple documents and spreadsheets scattered across departments and owners," suggests Brad Thompson, manager of Special Projects & Lean initiatives for Hendrick. "By leveraging our PPM system, we are now able to ensure the right people are working on the right projects," he adds. In a large healthcare setting, it is not uncommon to have several areas working on the same initiative without even knowing it. Even worse, a health system could have departments actually working against one another trying to achieve the same outcome.
When Hendrick combined its PPM launch with Lean training, the organization found initial users were not immediately documenting their key activities within the application, an indication it may have been too much to absorb at one time. "We will be focusing on improving our adoption going forward and hope to demonstrate comparable financial results to other organizations that have started before us," adds Bessent.
Grady Health System (Atlanta)
62 Active Projects, 14-20 new ideas added each month
With 918 beds in its main campus facility, Grady Health System includes the largest hospital in the state of Georgia and the 35th largest in the U.S. "The greatest challenge facing health systems like Grady is remaining steadfast in our journey from volume to value, while remaining mindful of how this impacts definitions and measurements of quality," argues Raymond Smith, Grady's director of clinical decision support. "Tracking our ongoing performance improvement initiatives is vital as we continue to evolve in this direction."
Rising to this challenge, Grady embraced Project Portfolio Management about a year ago as a means of aligning quality and performance improvement strategies. As a result of this and similar investments, Grady Health System has shown demonstrable success in driving efficiencies that are unprecedented in typical safety-net organizations.
Key PPM Metrics – Grady Health System
- 14 Active Project Leaders
- 17 Departments impacted by current projects
- 85 Projects in various stages of execution
- 45 Lean projects
- 32 A3 projects
- 5 PDSA projects
- 3 DMAIC projects
Grady's application of their PPM is the perfect embodiment of Wesbury's direction to not only do things right, but to also do the right things; Lean and A3 are straightforward methods for dealing with a majority of process improvement needs, while DMAIC (standing for define-measure-analyze-improve-control) is the method employed for the most complex of situations.
"Our PPM makes it easy to access powerful tools from each methodology, combined with cloud-based dashboard reporting, allowing us visibility into the progress of all initiatives," claims Smith. "We could not achieve these levels of performance without the benefit of a PPM."
Conclusion
To be sure, no amount of technology is going to make it easier for CEOs to sleep at night, content in the knowledge that their system is on track to exceed their performance targets. Adequate adoption of PPM and the technologies they propagate will require that organizations emphasize to staff all the benefits these systems are capable to provide: better collaboration, more transparency and tighter accountability. Of course, not everyone will embrace being held more accountable. But to avoid accountability is tantamount to sub-optimizing your organization's potential.
In the end, like many other proven approaches to performance improvement, PPMs are likely to separate winners from losers in the rush to adapt to the ever changing landscape of industry.
Ian R. Lazarus FACHE is President and CEO of Creative Healthcare, a company supplying training in Lean, Six Sigma and Emotionally Intelligent Leadership. CHC also offers the COMPASS® Quality Management System, a PPM for health systems and industries dedicated to continuous improvement.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker's Hospital Review/Becker's Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.