The proposal for Stage 3 of the Meaningful Use Incentive Program, published March 30, 2015, represents what could be a sea change in how EHR and practice management software systems operate, especially concerning interoperability.
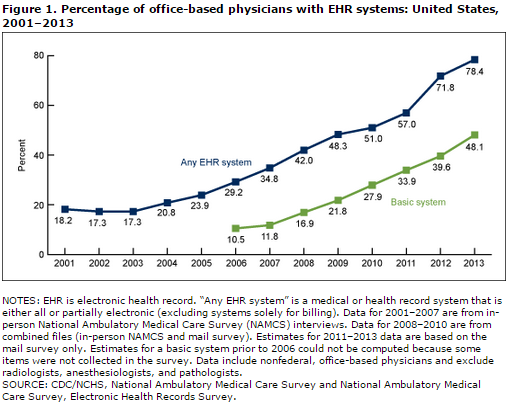
Though electronic medical records (EMR) were in use long before they were "meaningful," it's difficult to imagine what healthcare IT would look like without Meaningful Use. The CMS's flagship incentive program has driven the adoption of electronic health records across the nation. According to the Department of Health and Human Services, over half of eligible doctor's offices and 80 percent of hospitals had adopted an EHR system by the end of 2013, with over 535,000 eligible providers and hospitals having registered for the incentive program as of March 2015. Data concerning EHR/EMR adoption prior to the incentive program is spotty, but the CDC chart below tracks adoption over a twelve-year period. The beginning of the incentive program in 2011 caused a very clear jump — from 57 to nearly 72 percent adoption in a single year.
This growth has continued despite issues with many current healthcare IT systems. For every EHR success story, there seem to be a counter tale. Interoperability — or the lack thereof — is a common concern, but that may soon change. Perhaps the most exciting component of the new proposed rule is the inclusion of the "new" objective concerning patient access to electronic health information. Previously, as part of Stage 2 requirements, at least five percent of patients were required to view, download, or transmit their protected health information by interacting with their physician's patient portal. Stage 3 proposes to remove the specificity in method and minimum threshold, instead requiring that all patients must be able to access their health information electronically, and preferably through use of an application-program interface (API). As of press time, in the proposed rule's current form the API proposal is optional, but CMS is seeking comment from providers on whether or not it should be made a requirement. It should.
If the goal is true semantic interoperability, HL7-friendly APIs should have been required of every EHR at the beginning of the incentive program. Unfortunately they weren't, and now EMR vendors frequently deny any outside access to their data, or charge exorbitant amounts of money for tasks that should be simple. Using an API, even a programmer with minimal experience could interface EHRs from disparate vendors. The failure to include this as an initial requirement has resulted in horror stories such as an EMR vendor holding a hospital's records hostage when they switched programs, and other monopolistic practices from some of the nation's largest vendors. Furthermore, the lack of accessible APIs or similar resources has likely prevented a great deal of innovation in healthcare devices, services, and service delivery.
Consider Salesforce, the industry-leading customer relationship management platform. Instead of locking up their platform and discouraging development of third-party applications or interfaces, Salesforce built a marketplace and published their API. This has encouraged developers to create one of the largest business software ecosystems ever, with little to no investment from Salesforce themselves. Contrast this with the approach of a company such as Epic, that up until recently only offered limited data exports through their own proprietary service. Though they've recently announced an application exchange of their own, it remains to be seen how easy it will be to access and use any API Epic develops.
APIs will be the real catalyst for changes in healthcare IT, but another proposed objective should improve the experience of patients and providers everywhere: more than 15 percent of unique patient records should include patient-generated health data from a non-clinical setting. This could include health or care-related data from nutritionists, physical or occupational therapists, psychologists, home health providers, or even self-monitoring data from wearable trackers or manual recording of vitals. Many patients may not care too much about this. But for engaged patients, especially those managing chronic illnesses with tracking devices, this could greatly improve their experiences with providers, and their overall health. APIs can play a role here as well; it will be far easier to integrate wearable devices, personal health records, or other sources of patient-generated health information using an open API.
Last but certainly not least, if APIs are required and EHR data becomes more accessible to patients and other providers, the development of better telemedicine applications shouldn't be too far behind. A doctor performing a telehealth consultation could access a patient's health history from their primary care physician's EHR, an affiliated health information exchange (HIE), or other data source. That means they'd have access to more complete, better information, and care outcomes would likely improve accordingly. Furthermore, patients could more easily maintain and ensure the accuracy of their own personal health records, and make them available to all providers involved in their care.
Despite some disillusionment with previous iterations of the Meaningful Use Incentive Program, the Stage 3 proposed rule should finally bring about the promise of health IT — semantic interoperability and improved population health modeling and management. Of course, as of press time, the rule has yet to be finalized, so it's entirely possible — perhaps even probable — that CMS will not require vendors to include APIs. If that occurs, it will be interesting to see how the market reacts once incentives are removed. APIs make the most sense from the standpoint of interoperability and long-term platform viability; a vendor that doesn't offer an API should not survive in a fair marketplace when competing with vendors that do.
Charles Settles is a product analyst at TechnologyAdvice. He covers topics related to marketing automation, healthcare IT, and project management. Connect with him on LinkedIn.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker's Hospital Review/Becker's Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.

