Trustees and board members rely upon internal audit and compliance work plans in mitigating risk. Hospital executives should ensure that healthcare reform provisions, such as value-based purchasing, are considered in the development of annual internal audit and compliance work plans. This article will discuss the risks arising from Medicare's new Value-Based Purchasing program.
What's it all about?
On May 6, 2011, CMS issued the final rule related to VBP. This program was in development for more than six years prior to its implementation in federal fiscal year 2013. VBP is based on the premise that by improving the quality of patient care in the hospital setting, Medicare can mitigate the significant financial consequences of readmissions and adverse events.
FY 2013 hospital quality performance scores are based on 12 Clinical Process-of-Care measures (derived from patients' medical record documentation) and on eight Patient Experience of Care measures (derived from patients' responses to standardized surveys). Much of this information is publicly reported on the Hospital Compare website. Specific CPC measures are expected to change from year-to-year as each measure's performance improves. In FY 2014, the VBP measures will also include efficiency measures, such as "Medicare spending per beneficiary."
The VBP incentive payments are based on how well the hospital performs on these two sets of measures (achievement score), or how much the hospital improved their performance on each measure as compared to their performance during a baseline period (improvement score). CPC scores account for 70 percent of the hospital's Total Performance Score, while Patient Experience of Care scores account for 30 percent.
The Office of Inspector General 2012 Work Plan included a project to "review hospitals' controls for ensuring the accuracy and validity of data related to quality of care that they submit to CMS for Medicare reimbursement."
Internal audit testing should address the following:
As healthcare reform measures are implemented, trustees, board members and CEOs should verify that internal audit and compliance work plans address the associated risks.
Cindy Dupree, CPA, FHFMA, CCS, is a partner in Draffin & Tucker LLP's Audit and Accounting service group in Albany, Ga., where she focuses on the healthcare industry. She is also director of consulting and compliance Services for the firm. Ms. Dupree has more than 40 years of accounting experience, including charge description master reviews, community health needs assessments, community benefit planning, compliance programs, revenue cycle improvement and various operational and reimbursement projects. She is a frequent speaker to healthcare organizations, including HFMA and hospital associations, as well as in-house seminars to individual hospitals
Medicare value-based purchasing
Under Section 3001 of the Patient Protection and Affordable Care Act, Medicare established the VBP program. Beginning Oct. 1, 2012, hospitals are paid not only for the volume of services performed, but also for the quality of care provided. Quality is measured using information taken from the patient's written medical record documentation and from survey information provided by the patients after discharge.What's it all about?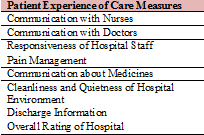
On May 6, 2011, CMS issued the final rule related to VBP. This program was in development for more than six years prior to its implementation in federal fiscal year 2013. VBP is based on the premise that by improving the quality of patient care in the hospital setting, Medicare can mitigate the significant financial consequences of readmissions and adverse events. How does it work?
Each hospital paid under the Medicare Inpatient Prospective Payment System methodology experiences a "withhold" from its Diagnosis-Related Group payments. Medicare then pools this withhold amount and redistributes the funds to those hospitals with high quality performance scores. The higher the hospital's performance score, the higher the incentive payment the hospital receives. The withhold amounts gradually increase from 1 percent in federal FY 2013 up to 2 percent in FY 2017 and thereafter.FY 2013 hospital quality performance scores are based on 12 Clinical Process-of-Care measures (derived from patients' medical record documentation) and on eight Patient Experience of Care measures (derived from patients' responses to standardized surveys). Much of this information is publicly reported on the Hospital Compare website. Specific CPC measures are expected to change from year-to-year as each measure's performance improves. In FY 2014, the VBP measures will also include efficiency measures, such as "Medicare spending per beneficiary."

The VBP incentive payments are based on how well the hospital performs on these two sets of measures (achievement score), or how much the hospital improved their performance on each measure as compared to their performance during a baseline period (improvement score). CPC scores account for 70 percent of the hospital's Total Performance Score, while Patient Experience of Care scores account for 30 percent.
The role of internal audit and compliance
In FY 2013, 70 percent of each hospital's quality performance score for VBP incentives is based on data derived from hospital records. The use of internally generated hospital data in computing VBP scores creates not only new areas for governmental scrutiny, but also new opportunities for monitoring by hospital internal auditors and compliance officers.The Office of Inspector General 2012 Work Plan included a project to "review hospitals' controls for ensuring the accuracy and validity of data related to quality of care that they submit to CMS for Medicare reimbursement."
Internal audit testing should address the following:
- Does the hospital have controls in place to ensure the accuracy and validity of the quality data submitted?
- Have the controls been tested to ensure effectiveness?
- Do the controls ensure that medical records contain documentation to support adherence to the CPC measures?
- Do the controls ensure that all patient records meeting diagnoses criteria are included in quality reporting?
- Do the controls to ensure all eligible patients are receiving HCAPHS surveys?
- Compliance officers should test the validity of the quality measures reported.
- Validate that hospital medical records contain documentation to support CPC responses.
- Validate that all eligible patient records were queried in CPC reporting.
- Validate that all eligible patients were included when sending HCAHPS surveys.
As healthcare reform measures are implemented, trustees, board members and CEOs should verify that internal audit and compliance work plans address the associated risks.
Cindy Dupree, CPA, FHFMA, CCS, is a partner in Draffin & Tucker LLP's Audit and Accounting service group in Albany, Ga., where she focuses on the healthcare industry. She is also director of consulting and compliance Services for the firm. Ms. Dupree has more than 40 years of accounting experience, including charge description master reviews, community health needs assessments, community benefit planning, compliance programs, revenue cycle improvement and various operational and reimbursement projects. She is a frequent speaker to healthcare organizations, including HFMA and hospital associations, as well as in-house seminars to individual hospitals
More Articles on Value-Based Purchasing:
Which Hospital Markets Had the Best 2013 Value-Based Purchasing Results?
CMS Announces Value-Based Purchasing Winners, Losers

