Editor’s Note: This article is the second in a 3-part series. The first article “Making the Decision” can be found here.
After all, the benefits can include an opportunity to drive operational improvements, tighter alignment with physicians and additional incremental volume. The decision to pursue bundled payments is only the first step, however. The second step — selecting the right service(s) to bundle — is critical to ensuring the success of a bundled product. This article presents a how-to guide for selecting the ideal bundled service.
Defining selection criteria
Cleveland Clinic has created a cardiac surgery bundled program. Johns Hopkins has developed a joint replacement bundle. Each of these programs was undoubtedly informed by in-depth analytics and a thorough evaluation of pertinent market factors. While every organization is different, selecting the right service to bundle requires a systematic assessment of strategic, financial and operational criteria.
Strategic criteria
– Market conditions — Market (payors and patients) demand and the presence of competitor bundles/payor partnerships
– Physician alignment — Physician willingness to participate in a bundle (e.g., care protocols, patient care management) and agreement with financial incentives
Financial criteria
– Utilization variance — The ability to reduce variation, optimize utilization and generate cost savings that drive the contribution margin and potential shared savings pool
– Contribution margin — The contribution margin and reimbursement level to meet organizational targets
Operational criteria
– Clinical quality — A demonstration of high-quality clinical care for contract discussions and marketing purposes
– Care management capabilities — Skill and experience in clinical care management to optimize utilization and manage the risk of the patient population
Health systems should prioritize these criteria based on internal factors, including the alignment of the bundle with the organizational vision, the overall strategic importance of the service line, and the bundled program’s relationship to other strategic initiatives, such as an accountable care organization. If a bundle is developed in a service line that doesn’t coincide with a strategic initiative, the organizational support that the bundle receives will be limited.
Strategic criteria
Payors and patients alike are seeking healthcare options that provide strong value with high quality. To offer a bundle to meet demand in the market, health systems require careful planning and analysis that will vary according to the specific bundled episode. It is necessary to critically examine the prevailing market conditions, as outlined below, for a bundled program under consideration.
– Current market share for the episode of care — Services with low market share may not have the volume necessary to demonstrate high quality and the potential for utilization savings. High market share services may be limited in their potential incremental volume and financial impact.
– Payor interest (both health plans and self-insured employers) in the episode of care — Payor interest in innovative reimbursement mechanisms could be minimized by factors such as a payor’s generally dominant market position or a low volume of patients with the proposed episode of care.
– Competitor bundle activity and offerings in similar or related services — A health system in a highly fragmented market may offer a bundle as a market differentiator to develop a competitive advantage. Conversely, markets with directly competing bundles can exacerbate rivalry for physician alignment and deflate reimbursement without the expected incremental volume increases.
– Physician alignment in the market — Physician relationships are critical because they drive the utilization and cost-savings efforts. The level of current or desired alignment with physicians is recognized by multiple sources as a critical component to having a successful bundle.
Financial criteria
There are two methods to achieving financial success through a bundled program: the first is capturing incremental volume, and the second is creating savings in both the cost of care delivery (i.e., improving the contribution margin) and the average utilization (i.e., improving the shared-savings pool). To meet one or both of these goals, an organization must understand the following:
– Utilization variation among patients/providers — Episodes of care that currently exhibit a high variance in cost or patient utilization provide the best opportunity for generating utilization savings as well as cost savings. A reduction in variation is achieved through physician adherence to protocols and other measures.
– Price relative to competitors — Payors are more willing to work with health systems to direct volume through benefit design if per unit savings can be achieved. High relative prices could also be suppressing volume for a given provider.
– Care delivery costs — The delivery costs impact overall margin. Bundles that offer a slight discount to a payor can still be successful if the health system is able to achieve some further delivery cost savings to maintain high margins. It is important to note that many of the delivery cost savings are directly related to capacity and that savings in costs require additional volume or backfilling of capacity to be of true value to the health system.
– Contribution margin — The contribution margin after discounts and cost savings should be reviewed by the finance team. Offering a bundle that decreases the margin may be a poor choice for the health system.
– Bundle scope — The scope of the desired bundle, including service exclusions and time period, directly impacts the utilization risk and the potential for additional spend. The additional spend in turn negatively impacts the overall cost of care and average spend per patient, thereby eroding the prospective payment or available shared savings.
– Patient Risk Profile — Patient risk factors and comorbidities introduce more variance that can have negative financial impacts. A bundle that includes a broad scope of service and few patient exclusions can increase the potential financial reward by adding volume and reimbursement. However, riskier patients increase variation and can eliminate savings with one or two bad outcomes.
Operational criteria
The best bundled options are those that exhibit strong quality performance relative to the market, and high quality is commonly achieved through effective and efficient operations that result in a consistent patient experience and clinical outcomes. Exceptional quality has two advantages: the first is the impact on utilization and variability. A high-quality service with a consistent protocol limits negative outcomes and unnecessary utilization. The second advantage is that organizations can use their demonstrated high quality as a marketing tool. A high-quality service can function as a central theme to draw patients from an expanded market. Executing the highest-quality bundled service requires operational skill in the following areas:
– Clinical protocols — Many health systems have developed protocols for their highest-volume procedures. An established care process that is adopted by the care management team for the desired episode bundle brings consistency. A care protocol, either new or existing, is a requirement for a successful bundle.
– Care management — A health system’s ability to manage the cost continuum is important for optimizing utilization. The care management team must be comfortable with not only evaluating the medical necessity of the service but also managing the use of the service and directing care to appropriate in-network providers. Care management can include pharmaceuticals, and the use of generic medications, and extend to the proper utilization of preferred vendors or other services.
– Bundle tracking — Tracking bundle patients and reporting relevant metrics are two elements that are often overlooked. Health systems need to support the care management team with the ability to monitor the performance of bundle patients versus non-bundle patients. The appropriate billing for these patients also impacts patient satisfaction, another component of quality.
Organizations should review the criteria in these three areas (strategic, financial and operational) before selecting the best option for a bundled payment program.
Evaluating an example
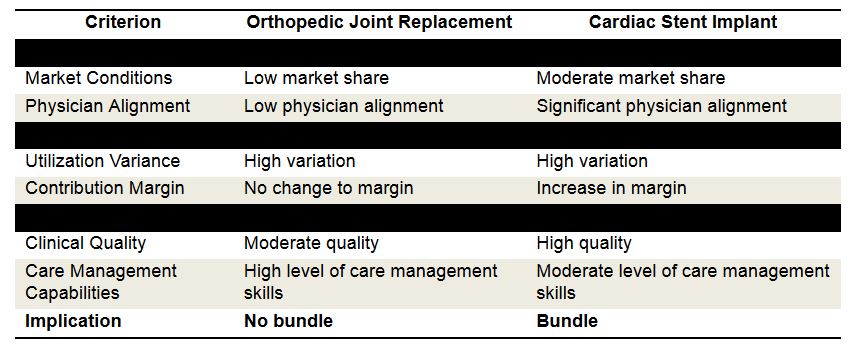
The table below summarizes how the selection criteria could be applied at a high level in a given market for possible bundles at an example hospital.
Jason Lee is a senior manager with ECG. In more than a decade as a healthcare industry consultant, Jason has worked with health systems nationwide to create hospital/physician alignment structures and optimize innovative reimbursement mechanisms. He is a nationally recognized speaker on managed care and health exchange issues.
Josh Neal is a manager with ECG. Since joining ECG in 2010, Josh has assisted clients in executing a wide range of hospital/physician alignment models, implementing accountable care/clinical integration programs and developing the capabilities required for success under value-based payment arrangements.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker’s Hospital Review/Becker’s Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.