Call it what you may — ACO, ACE or CCO — Medicaid accountable care and care coordination initiatives are on the rise. State-supported care coordination activities, patient-centered medical homes, value-based payment arrangements and quality improvement initiatives are expected to increase steadily in 2014.
Oregon, Colorado and Utah have the most established Medicaid accountable care programs, and states like Illinois and Minnesota recently legislated support as well.
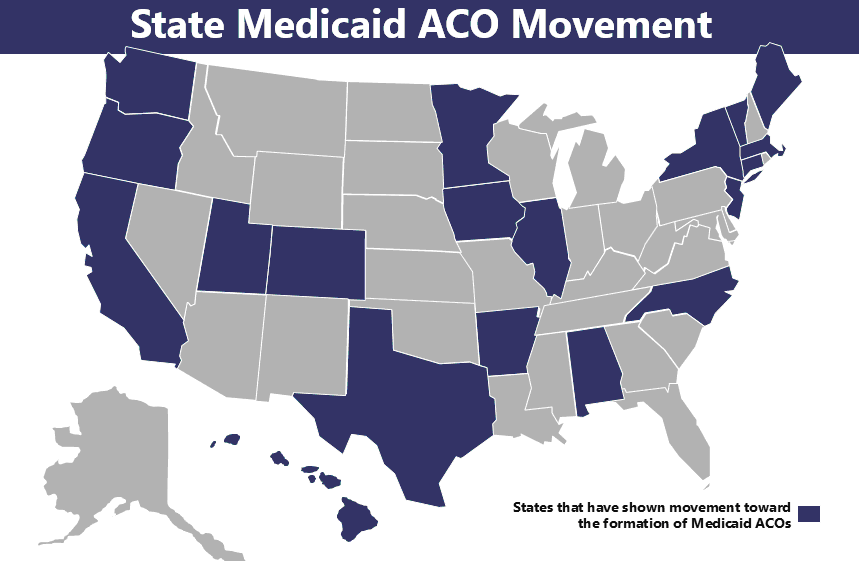
For simplicity sake, I will refer to various state Medicaid accountable care initiatives as ACOs. The following chart demonstrates the broad state support for Medicaid ACOs:
While the Medicaid ACO movement is broadly supported, no two state initiatives are alike. For example, the State of Illinois, which calls its ACOs, Accountable Care Entities, has mandated that any ACE must include primary care, specialty care, hospitals and behavioral healthcare, and must have a governance structure that includes each type of provider. The ACEs must participate on a three-year path to move away from the current fee-for-service structure, which includes: (1) shared savings during the first 18 months, (2) partial risk after 18 months and (3) full risk after three years. The ACEs are also expected to construct a supporting infrastructure that includes health information technology, risk assessment tools, data analytics and communication with Medicaid members. 1
North Carolina plans to construct a budget model for each state ACO, and providers can share in any savings achieved if they improve health outcomes. Providers are also on the hook for shared losses if costs exceed the benchmark. North Carolina's proposed ACO legislation, if implemented, could reduce the state's $13 billion Medicaid spending by 3 percent or several hundred million dollars. 2
The State of Oregon, perhaps the most advanced and operational of all State Medicaid ACOs, has formed a total of 16 Coordinated Care Organizations, which cover over 750,000 lives. Before their CCOs, Oregon separated physical, behavioral and other types of care. Oregon has since incorporated a patient-centered and team-focused care delivery system that encourages better coordination and focuses on prevention, chronic disease management and patient-centered medicine. As a result, Emergency Department visits by people treated at CCOs have dropped 13 percent since 2011. The CCOs also lowered hospital admissions for congestive heart failure by 32 percent, chronic obstructive pulmonary disease by 36 percent and adult asthma by 18 percent. Spending for primary care is also up 18 percent.3
Why should high-level hospital leaders, including CEOs, CFOs, COOs and CIOs be following local state- level Medicaid ACO initiatives? Medicaid ACOs are not synonymous with managed Medicaid. Medicaid ACOs are taking a broader approach to patient care by focusing on population health and integrating services beyond the physical health components.4 For example, mental health, chemical dependency and dental services could all be covered as they are in Oregon.5 Medicaid ACOs are also encouraging a greater assumption of provider risk — sometimes in the form of shared savings with downside risk as it is proposed in North Carolina.6
State Medicaid activity can also encourage a local culture that embraces private and Medicare backed accountable care initiatives. The more investment and resources that organizations put into care coordination, the greater the spill-over potential will be for local accountable care activity.
For example, Camden, N.J., is home to the Camden Coalition of Healthcare Providers, and is one of the largest and most well-known Medicaid ACOs in the country. The Coalition involves Cooper Health System, Virtua Health, Our Lady of Lourdes Medical Center and multiple independent providers. Cooper has also formed its own commercial ACO and Virtua signed up with the MSSP ACO round 3 cohort. In fact, Virtua is involved in four overlapping efforts: a Medicare ACO with CMS (12,000 covered lives), its own ACO through a self-insurance plan for employees, a Medicare Advantage ACO with Aetna (1,100) and a pending project with a commercial payer (14,000). Beyond that, Virtua treats some 150,000 patients through its medical home effort.7
While the jury is still out on the efficacy of various State-sponsored Medicaid ACOs, few people would question the impact the Medicaid ACO movement is beginning to have across the country. Even though MSSP and Pioneer ACOs have received the lion's share of press attention, Medicaid ACOs will play a vital role in shaping local market dynamics.
Douglas Hervey conducts leading-edge intelligence at Leavitt Partners on the accountable care movement through national tracking and monitoring of ACOs. He has also worked for innovation expert Harvard Business School Professor Clayton Christensen on ACO expansion and collaborated with a number of healthcare and technology startups.
1 Accountable Care Entity (ACEs). Retrieved from https://www2.illinois.gov/hfs/PublicInvolvement/cc/ACE/Pages/default.aspx
2 DeBruyn, Jason. (2014, Mar. 17). New N.C. Medicaid reform plan would trim 3% off the $13 billion budget. Retrieved from http://www.bizjournals.com/triangle/news/2014/03/17/medicaid-reform-would-save-3-percent-off-the-13.html
3 Oregon’s Health System Transformation. Quarterly Progress Report (2014, Feb) http://www.oregon.gov/oha/Metrics/Documents/report-february-2014.pdf
4 Accountable Care Entities (ACEs). Retrieved from https://www2.illinois.gov/hfs/PublicInvolvement/cc/ACE/Pages/default.aspx
5 Oregon’s Health System Transformation. Quarterly Progress Report (2014, Feb) http://www.oregon.gov/oha/Metrics/Documents/report-february-2014.pdf
6 DeBruyn, Jason. (2014, Mar. 17). New N.C. Medicaid reform plan would trim 3% off the $13 billion budget. Retrieved from http://www.bizjournals.com/triangle/news/2014/03/17/medicaid-reform-would-save-3-percent-off-the-13.html
7 VirtuaCare ACO. Retrieved from https://www.virtua.org/about/aco/default.aspx


