The majority of health systems have likely engaged in workforce planning, alignment strategy development, or both in the last few years. But how many have conducted these two processes simultaneously?
The benefits of approaching workforce planning and physician alignment in conjunction are numerous and can result in strategies that accurately reflect the true needs of the health system.
Health systems’ investment in their physician workforce is a critical factor for not only meeting the care needs of their communities but also positioning the systems to defend their market share and grow network adequacy. As health systems design their physician network alignment strategy, workforce planning plays a key role in its development, providing both a system and market view of provider needs. Recent trends reflect the value of the physician workforce to health systems, with new players in the physician group space (e.g., private equity [PE] firms, health insurance plans) posing a threat to the status quo and placing further impetus on health systems’ need to align closely with physician groups through employment or tight affiliation (e.g., PSAs, JVs).
Goals of Workforce Planning
Workforce planning for many health systems is a standard activity that takes place, on average, every three years. Beyond its role as a routine strategic planning process and regulatory requirement, workforce planning also achieves several key goals to support the development of the health system’s medical staff.
» Workforce planning provides a validated assessment of the hospital’s current medical staff composition relative to the overall provider community.
» Through a robust verification process, hospitals can collect and analyze critical data on panel size, payer access, and appointment wait times. Health systems then use comparative metrics and demographic analyses of the patient population to ensure the needs of the community are met with well-distributed services. They also determine which specialties may be vulnerable to attrition.
» Workforce planning allows a health system to examine gaps in the geographic distribution of physicians and advanced practice providers and identify where succession risks due to an aging workforce are greatest within its market.
Intersections between Workforce Planning and Alignment Strategy
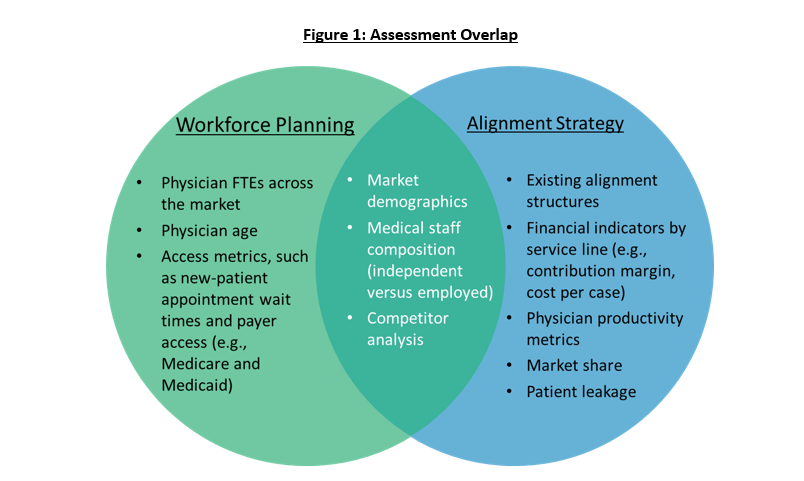
There are many intersections between workforce planning and alignment strategy development; conducting them in concert can provide great efficiencies to a health system. A foundational element of workforce planning is population-based demand calculations, where community need is expressed in net need for physicians at the market level. Similarly, evaluating population trends in a market is a basic exercise for any type of strategic planning, whereby understanding market dynamics can help inform decisions about where and when physician alignment should occur.
At the health system level, assessing need requires an understanding of the referral relationships and patient leakage out of the system and how additional market share can be captured. The overlap between community need and health system need can inform where alignment opportunities may be most desirable in certain specialties, particularly where market growth is considered as well as the age profile of the physician supply. Understanding future physician need enables health systems to develop a framework that supports the timing of alignment decisions.
Alignment strategies developed alongside routine workforce planning processes provide a holistic view of the physician market, and care should be taken to gather robust data that supports both objectives. Key elements of a workforce planning exercise may include:
» Composition of the medical staff.
» Access issues.
» Areas of community and system need.
There is extensive overlap in the data assessed as part of both processes, as shown in figure 1.
Applying an Alignment Framework
Typical alignment drivers could include practice retention, recruitment to support physician need and/or access, support for system-wide or service line strategic initiative(s), revenue enhancement, and medical staff diversification. Elements of both workforce planning and alignment can be assessed across all clinical service lines to evaluate the physician need and other relevant alignment drivers. Table 1 presents a few examples.
Table 1: Example Alignment Drivers
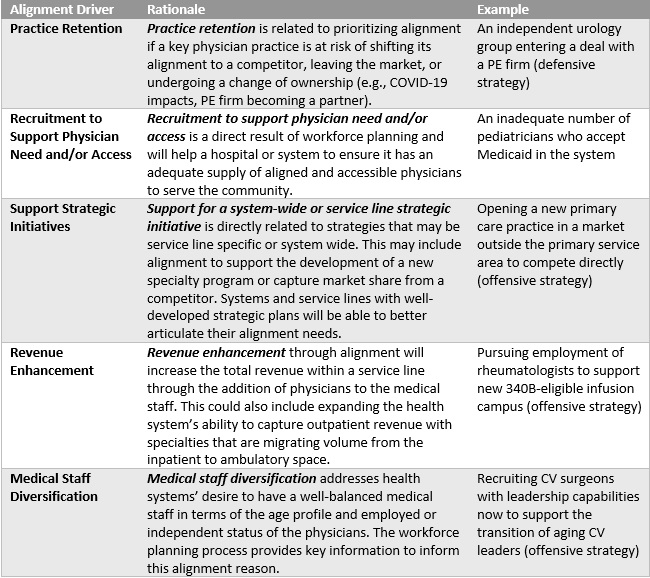
Evaluating the alignment drivers for a clinical service line, specialty, or specific physician group includes both objective and subjective qualitative analyses. However, a rigorous, data-driven analysis must be included in the evaluation of alignment drivers to comprehensively and objectively assess a given situation. The data-driven metrics utilized may vary greatly across health systems and are often dependent on the availability of data, market dynamics, and other health system–specific needs. Workforce planning–based metrics, such as the ratio of community need to health system need, will inform the recruitment driven by need and access.
» Specialties with a low community need but a high system need suggest alignment may be necessary to achieve network adequacy goals or bring the system closer to meeting the need of the community.
» Conversely, a high community need but low system need may suggest the system holds tight alignment with the physicians in the market and may not need to pursue additional alignment.
» Additionally, the age of the medical staff will inform the succession risk and guide the medical staff diversification driver.
These data points, in conjunction with a comprehensive analysis of the other alignment drivers, provide a foundation for alignment strategy development and prioritization.
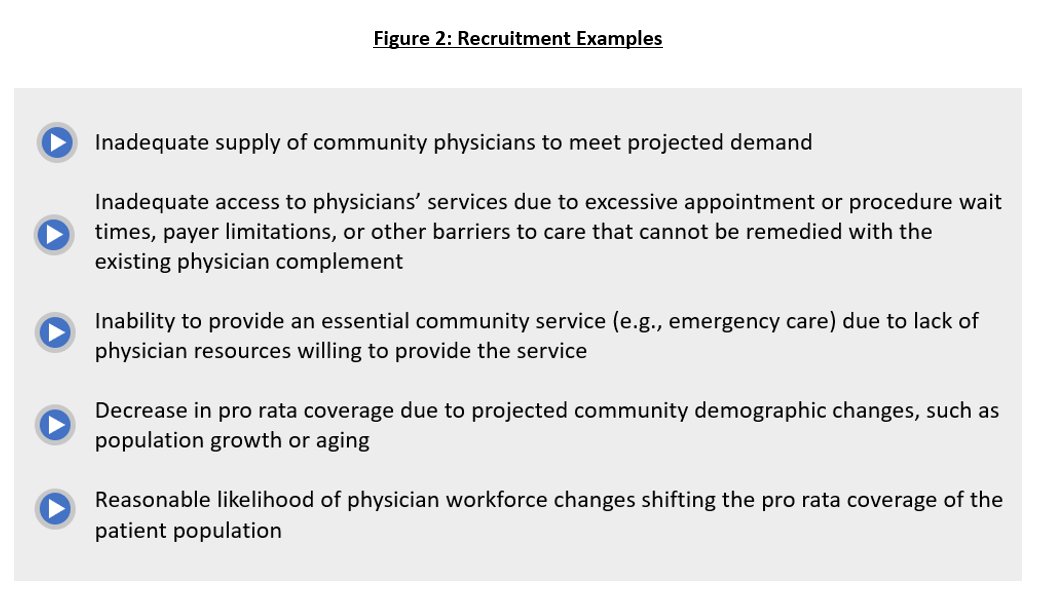
Legal Implications for Independent Practice Relationships
In addition to supporting the overall alignment strategy for a health system, workforce planning also provides insights into a health system’s ability to support recruitment for independent physician practices. Targeted recruitment support is one potential tactic often utilized in an alignment strategy. This type of recruitment may be legally permissible in the situations detailed in figure 2.
Final Thoughts
The number of intersections between workforce planning and alignment strategy supports the development of both in tandem. Sharing information, assumptions, and outputs between the two processes will bolster the overall alignment strategy for health systems. Workforce planning supports data-driven decisions that determine the prioritization of opportunities and the overall alignment strategy. Health systems that are evaluating their alignment strategy or their workforce planning should consider addressing them together to achieve economies of scale and ensure the most robust possible results that are supported by a data-driven analysis and structured decision-making process.
By Jennifer Moody, Emily Lopez, and John Lutz