Clinician engagement is linked in the literature to improvements in all four corners of the Quadruple Aim: patient experience, patient outcomes, cost of care, and provider experience.
Yet, today we focus on and hear much more about clinician burnout than engagement. A recent Medscape 2024 report reminds us that half of all physicians experience burnout. Taking the emergency medicine subset, nearly two-thirds of physicians report burnout.
As an antidote to burnout, we’ve been focused on clinician wellness. Though in practice, frequently this concept of wellness lands squarely on the shoulders of the individual clinician. Meditate. Take Yoga. Get counseling. Take a vacation. Take a deep breath. But, why focus on what the clinician must do? Simple, systemic solutions seem too challenging or costly – at least at first blush.
Let’s dig into this.
The psychological concept of engagement can help us understand opportunities for systemic solutions. In one systematic review, researchers unlock a definition of clinician engagement in the singular word "involvement". They decoded the process of involvement as one where a clinician is actively participating in:
- Deciding how one’s work is done,
- Making suggestions for improvement,
- Goal setting,
- Planning, and
- Monitoring of performance.
By involving clinicians in the systems in which they work, we realize improvements in care outcomes, patient satisfaction, cost reduction, and clinician wellness. It is worth taking a critical look at each of our systems to clarify where we have top-down dictation of clinician work, and where clinicians have been truly involved. It is also important to recognize that clinician involvement can occur at several levels within our health systems. The authors of this review identify three levels of activity: micro, meso, and macro. At the micro level are the day-to-day workflows; this is one of the most straightforward levels to identify activities for clinician involvement. At the meso level, involved clinicians are often emerging in healthcare settings as leaders, driving important change within the care delivery of that setting. And, at the macro level, we see clinicians taking part in health care systems beyond a single entity, participating in state or federal policy or addressing broader issues of public health. In the end, what matters is not the level of activity in which a clinician is involved, but simply their involvement in an activity.
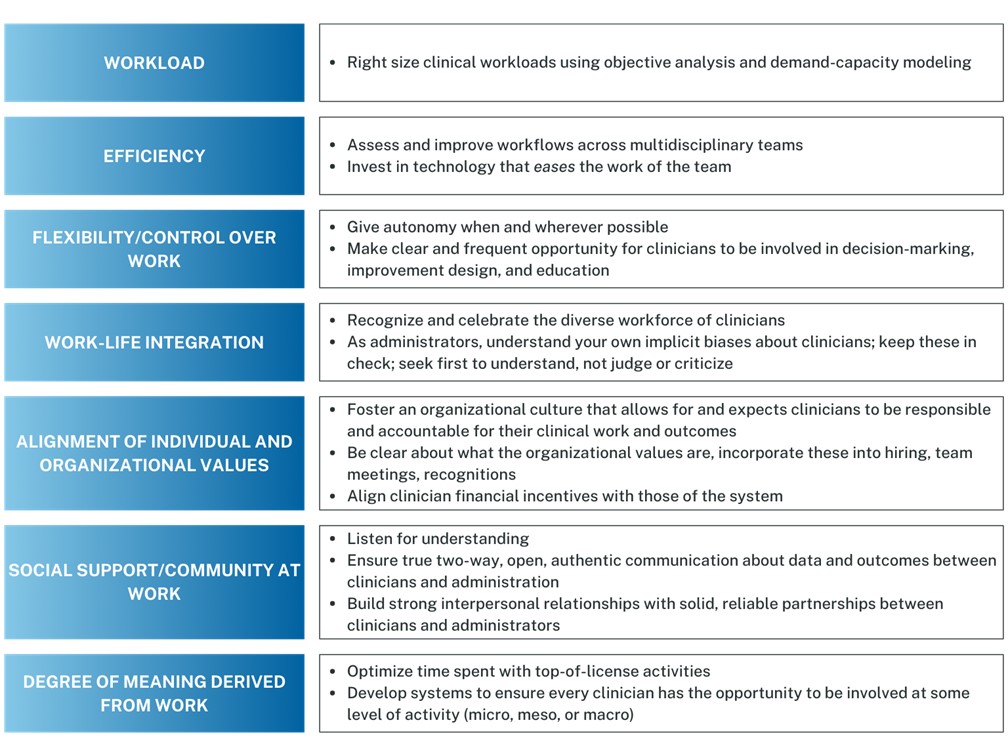
Breaking it down further, there are concrete, manageable system level opportunities for us to transform burnout to engagement. Shanafelt and colleagues identified seven important driver dimensions that help us identify options. These domains lead to burnout when things go poorly but lead to engagement when things go well. Within this framework, we identify several opportunities for systems to embrace changes and support clinician engagement. Figure 1 captures some of the ideas we’ve had success with at the systems level.
Figure 1. Driver domains and what systems can do to support clinician involvement and thus engagement.
None of this is rocket-science. Rather, it underscores what we need to remember: underneath it all, clinicians are human too. As with all things human, there is an art to developing a culture of engagement. From some of the most successful leaders, here are learnings we value in the practice of this art:
- Trust that clinicians want to do the right thing,
- Put the data in front of the clinicians and the clinicians in front of the decisions,
- Listening for understanding, make the time to truly listen, hone your skills to truly hear,
- Recognize people, yes for their good work, and even more for who they are as individuals,
- Begin with respect,
- Be consistent,
- Build trust and a sense of belonging,
- OVER communicate and,
- Be vulnerable and humble.
The transformation from burnout to engagement is not only possible but imperative for the well-being of clinicians and the sustainability of healthcare systems. By fostering a culture of engagement, we can enhance patient care and reignite the intrinsic motivation that drives clinicians. True progress lies in collaborative efforts, transparent communication, and a deep respect for the clinician’s role, ensuring that their voice is not just heard, but is influential in shaping the future of healthcare.


