The COVID-19 pandemic has stretched hospitals thin. Hospital leaders are now trying to understand how to leverage their remaining resources to rebuild and move forward.
At this point, hospital executives and boards could focus on any number of issues in finance, technology, and clinical operations. But before you pour time and energy into any initiatives, make sure you are focusing on the moves that will have the greatest impact in 2022 and the years to come.
Right now, effective leadership teams are concentrating on five strategic priorities.
1. Rebuilding your operating margin
Most hospitals tried to maintain profitability during COVID-19 by reducing staffing and service levels. These cost-cutting opportunities are now just about tapped out. Going into 2022, hospitals need to be more strategic about margin improvement.
One promising avenue is reducing unwarranted clinical variation. For example, implementing a standardized care pathway for heart failure patients with could significantly reduce average LOS, 30-day readmission rates and average adjusted direct costs.
To ensure strong operating margins, executive leaders and boards should make sure clinical variation reduction programs:
- Use trustworthy data and incorporate evidence-based standards
- Align clinical practices through a philosophy of continuous improvement
- Engage physicians in interdisciplinary teams that address the entire continuum of patient care
2. Recalibrating your surgery strategy
COVID-19 has accelerated the movement of procedural volume from hospitals to ambulatory surgery centers (ASCs). Disparities in site-of-service reimbursement are now having a major impact on hospital finances. Hospital leadership teams need to act decisively in 2022 to establish a perioperative strategy that addresses this shift from acute operating rooms to ASCs.
Start by crafting an integrated strategy that incorporates both your main OR and your outpatient surgery locations. Increasingly, the hospital OR should focus on complex surgical care while ASCs serve the consumer-driven market for common procedures. An understanding of the payers’ approach to contracting (and reimbursing) for procedures should play a big role in an integrated perioperative strategy.
In addition, take a careful look at your ASC investment philosophy. Is your hospital planning to build a new ASC? You should also consider investing in an existing facility or partnering with a national ASC development company. Each strategy offers a different opportunity in terms of costs and ROI.
3. Developing FFS alternatives
Insurance companies earned huge profits during COVID-19. However, few have shown any willingness to share their windfall in the form of increased fee-for-service (FFS) reimbursement.
Hospitals that are counting on FFS to drive recovery in 2022 face an uphill battle. The main source of any future revenue gains will be value-based contracts.
Hospital leaders must continue to develop their ability to take on risk and negotiate payer carve-outs for high-performing services. Leadership teams should also explore direct-to-employer (DTE) contracting. Provider organizations now have a strong opportunity to build revenue by creating “centers of excellence” that offer exceptional value to employers.
4. Cultivating your workforce
The impacts of the COVID pandemic placed tremendous pressure on the clinical and non-clinical workforce. This pressure adversely affected the progress of value-based care as it depends on full participation of physicians and clinical leaders. Unfortunately, many hospitals continue to lag in this area. Entering into 2022, executives and boards need to address workplace stressors, staff shortages, staff and physician burnout, and competitive workforce compensation.
Leaders should begin engaging physicians and middle-level managers through a formal governance and feedback structure focused on clinical process (re)design, workforce management, employee satisfaction improvements and program development with the ultimate goals of alignment and retention.
5. Building strategic partnerships
If there is an underlying theme to all these recommendations, it is this: Hospitals can no longer go it alone. To build value, negotiate effectively, improve patient care and increase revenue in the coming years, provider organizations need to form networks of strategic partnerships.
Community partnerships are essential to value-based care initiatives. They are also critical to responding effectively to healthcare consumerism. For example, hospitals now need to provide patients with a good virtual health experience. Health systems should consider partnering with a virtual primary care group to instantly create a strong telehealth/virtual health presence. This approach could expand your hospital’s geographic reach and improve patient access while strengthening referrals.
Implementation Tip: Set aside strategic time
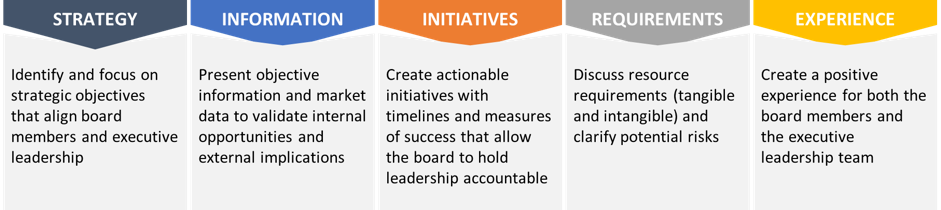
To take full advantage of these opportunities, hospital leadership teams should carve out dedicated time for taking a fresh look at long-term strategy. A facilitated board retreat is a very effective tool for resetting strategy and creating dynamic forward momentum.
To find out more and explore the possibilities for your organization, contact Daniel J. Marino or check out our INSIGHTS.