Reprinted with permission from the Association of Clinical Documentation Improvement Specialists (ACDIS) CDI Journal.
While many clinical documentation improvement programs try to measure the impact of their program and their clinical documentation specialists, there is still some confusion over how this is best measured. Consultants are eager to show that their efforts are benefiting the hospital, and CDI program managers are similarly motivated to show benefits to upper management. Inappropriate use of baseline metrics may be inadvertent, but can result in reports that show an inflated and unrealistic impact. This is compounded by the fact that many CDI programs leave the data analysis to an outside organization or software package, without understanding the origin or meaning of the data and metrics that are returned to them.
A CDI program should assist in creating medical documentation that most completely and accurately reflects the diagnoses, findings, treatments and outcomes of each patient. To fully measure and understand the workings of their CDI program, managers must strive to produce and report metrics that are brutally honest and insightful with regards to their department's activities.
Baseline DRG
This article focuses on the baseline metrics against which a CDI program can be evaluated. The first concept to explore is that of the baseline DRG, defined as the DRG that would have been coded and billed if no CDS was involved with the chart. The impact of a CDS's review and queries for a given patient admission is best thought of as the difference between the baseline DRG and the nilled DRG (while it is understood that the final Billed DRG produced by the coder may differ from that achieved by the CDS, we will assume they are the same for this discussion).
While the baseline DRG seems like a simple definition, this can at times be difficult to determine. Let’s take a sample clinical case to explore some of the issues:
The surgeon did not take the patient to the operating room based on the CDS query. And, the MCC that ultimately drove the reimbursement level was provided independently by the cardiology consultant, with no prompting from the CDS. Surprisingly then, the true financial impact that the CDS had on this case was $0! The documentation of the chronic kidney disease is, of course, important to the completeness and accuracy of the record on this patient, and severity of illness or risk of mortality may be affected. But claiming any direct financial benefit from the CDS involvement with this patient's documentation is not warranted.
Baseline case mix index (CMI)
So, the Baseline DRG is the DRG that would have been coded and billed without the intervention of the CDS. While not often done, the average weights of the actual baseline DRGs can be used to compute a case mix index, in an analogous fashion to using the average weights of the billed DRGs. In the sample chart below, the baseline CMI is shown with the red line, and the billed CMI, the one traditionally reported, is shown with the blue line. In the early stages of this CDI program, the difference between the two values appears to be due to the impact of the CDS, as we would expect. But notice that the baseline CMI is increasing over time, suggesting that the physicians are learning to document better. While the gap between the two lines, reflecting the CDS impact, narrows over time, the benefits seen in the billed CMI continue to be positive. While the interventional impact of the CDS may decline, a rise in the baseline CMI reflects the "training effect" of having a CDI program which cannot be discounted.
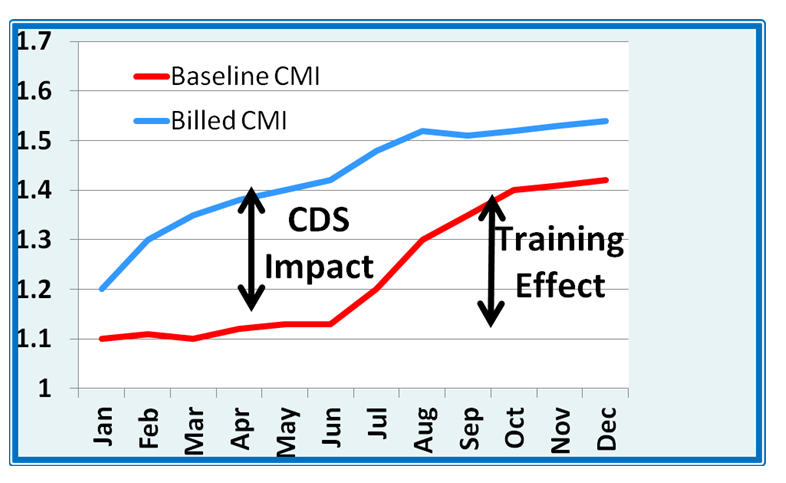
Selection of the baseline DRG should be done carefully, honestly, and precisely. You should be sure that you have control over the designation of the baseline DRG, or at least fully understand from where it is derived. You must be sure that your reports are not being artificially inflated by utilizing incorrect metrics or spreadsheet calculations, or you will not fully understand your program impact. Comparing the baseline CMI to the billed CDI can provide valuable insights into potential training effects on the physicians, and can help to identify opportunities for further education. Understanding the true impact of your CDI program is essential, and can only be done with accurate metrics.
With over 40 years of experience in computing and more than 25 years of experience in medical computing and information standards, Dr. Jonathan Elion, MD, FACC, has committed his career to innovations in high value services and healthcare delivery to maximize efficiency and cost effectiveness. Dr. Elion is the founder of ChartWise Medical Systems, Inc., a Rhode Island based company that recently introduced ChartWise:CDI. It is the first-to-market interactive software system designed to improve precision in quality clinical documentation and to support revenue assurance through its web-based, comprehensive built-in expertise, electronic queries and robust on-demand reporting.
Multi-Phased Approach, Engaged Physicians Lead to ICD-10 Success
While many clinical documentation improvement programs try to measure the impact of their program and their clinical documentation specialists, there is still some confusion over how this is best measured. Consultants are eager to show that their efforts are benefiting the hospital, and CDI program managers are similarly motivated to show benefits to upper management. Inappropriate use of baseline metrics may be inadvertent, but can result in reports that show an inflated and unrealistic impact. This is compounded by the fact that many CDI programs leave the data analysis to an outside organization or software package, without understanding the origin or meaning of the data and metrics that are returned to them.
A CDI program should assist in creating medical documentation that most completely and accurately reflects the diagnoses, findings, treatments and outcomes of each patient. To fully measure and understand the workings of their CDI program, managers must strive to produce and report metrics that are brutally honest and insightful with regards to their department's activities.
Baseline DRG
This article focuses on the baseline metrics against which a CDI program can be evaluated. The first concept to explore is that of the baseline DRG, defined as the DRG that would have been coded and billed if no CDS was involved with the chart. The impact of a CDS's review and queries for a given patient admission is best thought of as the difference between the baseline DRG and the nilled DRG (while it is understood that the final Billed DRG produced by the coder may differ from that achieved by the CDS, we will assume they are the same for this discussion).
While the baseline DRG seems like a simple definition, this can at times be difficult to determine. Let’s take a sample clinical case to explore some of the issues:
- The patient is admitted through the emergency department after presenting with abdominal pain, as-yet undiagnosed. While not optimal, this single symptom has a corresponding ICD-9 code (789.00), which would result in DRG 392, with a reimbursement at a "representative hospital" of $5,008.
- Further testing reveals that the abdominal pain is being caused by acute cholecystitis (ICD-9 575.10), which would result in DRG 446 (disorders of the biliary tract without complication), and reimbursement would be $5,175.
- The CDS notes an increased creatinine and a decreased glomerular filtration rate (GFR). A query is sent to the physician to clarify the renal status. If the physician documents it properly, it would be possible to assign a complication for Stage IV chronic kidney disease (ICD-9 585.4), which would result in DRG 445 (Disorders of the biliary tract with CC), and reimbursement would be $7,464.
- The patient undergoes a laparoscopic cholecystectomy (ICD-9 51.23), changing the DRG to 418 (Laparoscopic cholecystectomy with CC), with a resulting reimbursement of $11,868.
- The patient develops shortness of breath, and the consulting cardiologist documents acute-on-chronic congestive heart failure (ICD-9 428.23), changing the DRG to 417 (laparoscopic cholecystectomy with MCC), with a resulting reimbursement of $17,478.
The surgeon did not take the patient to the operating room based on the CDS query. And, the MCC that ultimately drove the reimbursement level was provided independently by the cardiology consultant, with no prompting from the CDS. Surprisingly then, the true financial impact that the CDS had on this case was $0! The documentation of the chronic kidney disease is, of course, important to the completeness and accuracy of the record on this patient, and severity of illness or risk of mortality may be affected. But claiming any direct financial benefit from the CDS involvement with this patient's documentation is not warranted.
Baseline case mix index (CMI)
So, the Baseline DRG is the DRG that would have been coded and billed without the intervention of the CDS. While not often done, the average weights of the actual baseline DRGs can be used to compute a case mix index, in an analogous fashion to using the average weights of the billed DRGs. In the sample chart below, the baseline CMI is shown with the red line, and the billed CMI, the one traditionally reported, is shown with the blue line. In the early stages of this CDI program, the difference between the two values appears to be due to the impact of the CDS, as we would expect. But notice that the baseline CMI is increasing over time, suggesting that the physicians are learning to document better. While the gap between the two lines, reflecting the CDS impact, narrows over time, the benefits seen in the billed CMI continue to be positive. While the interventional impact of the CDS may decline, a rise in the baseline CMI reflects the "training effect" of having a CDI program which cannot be discounted.
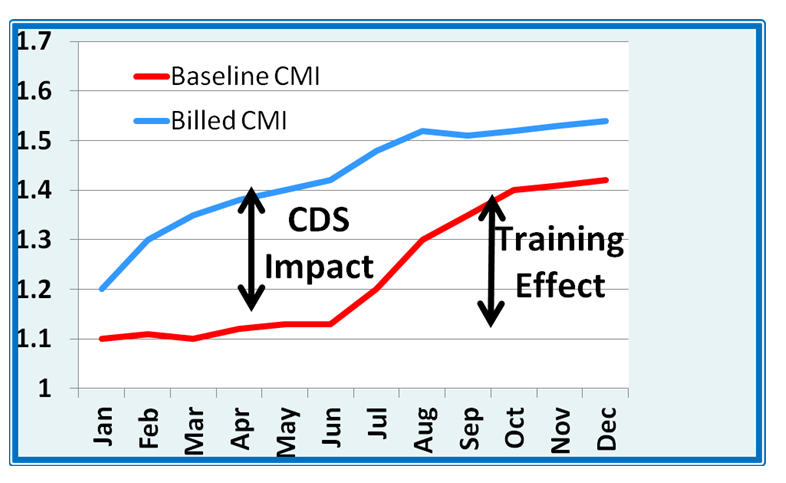
Selection of the baseline DRG should be done carefully, honestly, and precisely. You should be sure that you have control over the designation of the baseline DRG, or at least fully understand from where it is derived. You must be sure that your reports are not being artificially inflated by utilizing incorrect metrics or spreadsheet calculations, or you will not fully understand your program impact. Comparing the baseline CMI to the billed CDI can provide valuable insights into potential training effects on the physicians, and can help to identify opportunities for further education. Understanding the true impact of your CDI program is essential, and can only be done with accurate metrics.
With over 40 years of experience in computing and more than 25 years of experience in medical computing and information standards, Dr. Jonathan Elion, MD, FACC, has committed his career to innovations in high value services and healthcare delivery to maximize efficiency and cost effectiveness. Dr. Elion is the founder of ChartWise Medical Systems, Inc., a Rhode Island based company that recently introduced ChartWise:CDI. It is the first-to-market interactive software system designed to improve precision in quality clinical documentation and to support revenue assurance through its web-based, comprehensive built-in expertise, electronic queries and robust on-demand reporting.
Related Articles on Clinical Documentation:
Measuring Surgical Outcomes: Are Surgical Objectives Important Enough to Document?Multi-Phased Approach, Engaged Physicians Lead to ICD-10 Success


