A disturbing trend is on the rise for people who serve in a management capacity in healthcare.
It hit me when I read Overcoming the Peter Principle, by Andrea Ovans (2014). The Peter Principle is briefly defined as follows:
"The Peter Principle is a concept in management theory in which the selection of a candidate for a position is based on the candidate's performance in their current role rather than on abilities relevant to the intended role. Thus, employees only stop being promoted once they can no longer perform effectively, and "managers rise to the level of their incompetence."
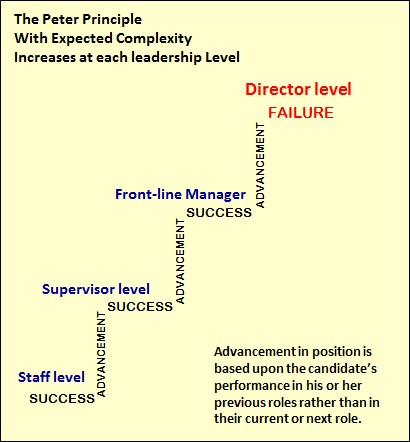
Figure 1. Visual demonstration where in theory, people advance to their level of incompetence based upon role complexity staying somewhat stable and consistent. (Attribution: Nevit Dilman / Wikimedia Commons / Public Domain)
We've measured and longitudinally tracked this trend as follows: People in Healthcare that serve in management at all levels are struggling at an accelerating rate that is unsustainable. This applies especially to the "B" level of overall effectiveness - a cohort of typically 50% to 60% of the entire management team.
The Facts
At Success Profiles, we have measured and tracked the overall effectiveness of people in Healthcare management since 2004. Our total sample size for this research includes over 30,000 people for one assessment tool and approximately 8,000 people for three other tools.
For years leading up to implementation of the Affordable Care Act, people in management performing in the "B" range that struggled in their role held steady, averaging approximately 16%. The "B" performance zone includes B-, B and B+ levels of effectiveness. "Struggling" is defined as missing the majority of performance outcome targets. In 2011 we observed an inflection point where rates skyrocketed to the 40% range - where we currently stand today. See Figure 2.
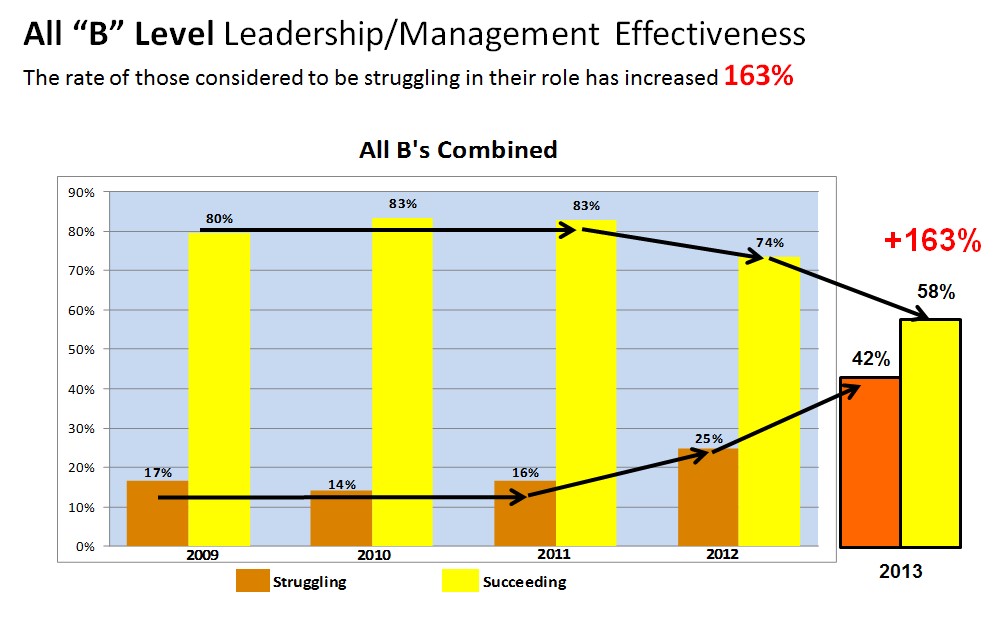
Figure 2. Illustration of the inflection point where the rate of all "B" level healthcare leaders struggling began to increase.
Our Hypothesis
What are the contributing causes? All evidence points to the fact that the overall portfolio of responsibility for management has significantly changed as a result of three major factors.
1. Degree of difficulty: The complexity of healthcare leadership assignments has increased abruptly. All people in management must take more ownership and be responsible for every aspect of "their business."
Vertically/functionally for front-line managers, performance expectations have changed dramatically. They now have to run a small business.
Horizontally for Director level leaders, the total number of departments/functions they lead increased due to "role creep" or a consolidation of management positions.
"Up and out" - Strategically for VP's and C-suite executives, managing external stakeholders (boards, business leaders, alliances, physicians, politicians, media, professional associations, GPO's etc.) has required more time than ever before. CEO's now spend up to 66% of their time managing "up and out" activities. Six years ago this was approximately 33% for CEO's.
2. The workload: Work quantity has reached the point of sub-optimized performance. Continued flattening of organizational management structures leaves more work on the backs of remaining leaders. See Figure 3.
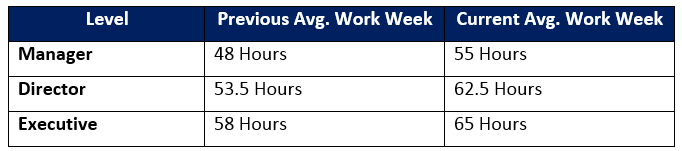
Figure 3. Average work week reported by leadership position.
Workloads create "Initiative Overload" when leader's lack "initiative priority discipline" to clearly differentiate between what seems urgent, what is most important and the actual capacity of the organization's management to truly manage major projects simultaneously.
Tony Schwartz captured this perfectly when he wrote, "even companies committed to creating positive work environments mostly continue to operate as if their people have infinite capacity, and are able to do ever more, with fewer resources. Precisely the opposite is true" (2014).
3. Underdevelopment: People have not "ratcheted up" their talent/demonstrated ability to manage the next level of responsibility fast enough, mostly due to insufficient investment in professional development. Every year, fewer financial resources are available for professional development and it is extremely difficult to measure the actual return on investment (ROI).
Professional development improvement takes longer than people think and does not occur very effectively with on-line learning. Degree of improvement is somewhat rate limited. People improve only so much. Not everyone becomes an exceptional leader even with unlimited investment of time and money.
In Figure 4, the left diagram illustrates the concept of the Peter Principle. The right diagram illustrates the impact that increasing complexity can have when the degree of difficulty of the assignment changes dramatically in a relatively short period of time.
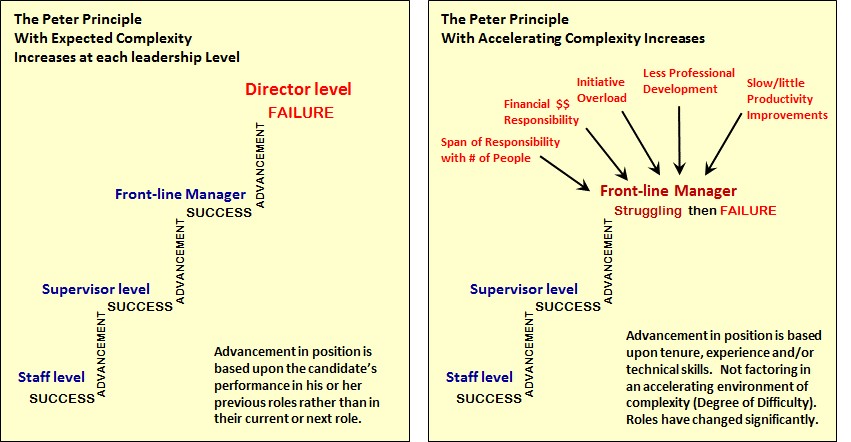
Figure 4. Demonstrating How the Peter Principle Gets Accelerated.
Inventory of Solutions
The following initiatives to consider align with an overall protocol of Leadership Alignment and Talent Management steps:
• Defining what talent is (demonstrated ability)
• Discovering where the talent is within the organization
• Developing and investing disproportionately in people who are Hi Performing (Hi-Per) and have High Potential (Hi-Po)
• Deploying the right people in the right Roles (RPR2)
1. Develop a whole new paradigm of leadership development (aka OD). Consider that a Healthcare system doesn't really produce a product, it is the ultimate service business. The organization must produce capable people who are effective at managing complex portfolios of services. Their ability to produce people to serve in management should be considered the equivalent of a Research and Development (R&D) investment. With an R&D budget mindset, how effective is the HR function in managing this process and is there a measurable ROI? Also consider where money is invested. Remember, your organization is not in the business of trying to develop everyone for management.
2. Have an objective process to evaluate people's demonstrated ability (e.g. strengths, struggles, competencies/skills, emotional intelligence and behavioral style intensities). Differentiate performance levels with everyone in management. You cannot possibly understand what improvements people need to focus on if you don't have an objective process to identify, measure and compare their management effectiveness to begin with.
3. Take inventory with how successful your organization has been with previous management appointments. Analyze over the past five years the following:
a. How many people have been appointed into a management role from inside and from outside the organization?
b. Overall, how effective have internal and external appointments been (total excelling, succeeding, struggling or failing)?
c. What is the ratio of inside vs. outside management appointments? The ideal range is somewhere between 66% and 75% internal appointments over a long period of time.
d. Are there common denominators or patterns for those that are successful and those that are not successful?
4. Identify which leaders are in over their heads (i.e. overleveraged and struggling). Help them improve. If they cannot sustain a consistent level of expected performance after about nine months of effort, find them a better role where they will more likely succeed. They are most likely a "good person" that has been "miscast." It is a disservice to leave them in a role where they will fail.
5. Identify and develop Hi-Per and Hi-Po leaders by creating a personalized career-path development plan and invest in them disproportionately. They represent the next generation of leaders that will navigate healthcare reform challenges and take the organization to the next level. Consider forming a formal mentoring program.
6. Avoid appointing new people into roles where they will be in over their heads to begin with. Consider their odds of success. Create guiding principles such as: Never appoint anyone below the "B+" level of demonstrated effectiveness into a high degree of difficulty assignment because their odds of success can fall below the 50% level. See Figure 5.
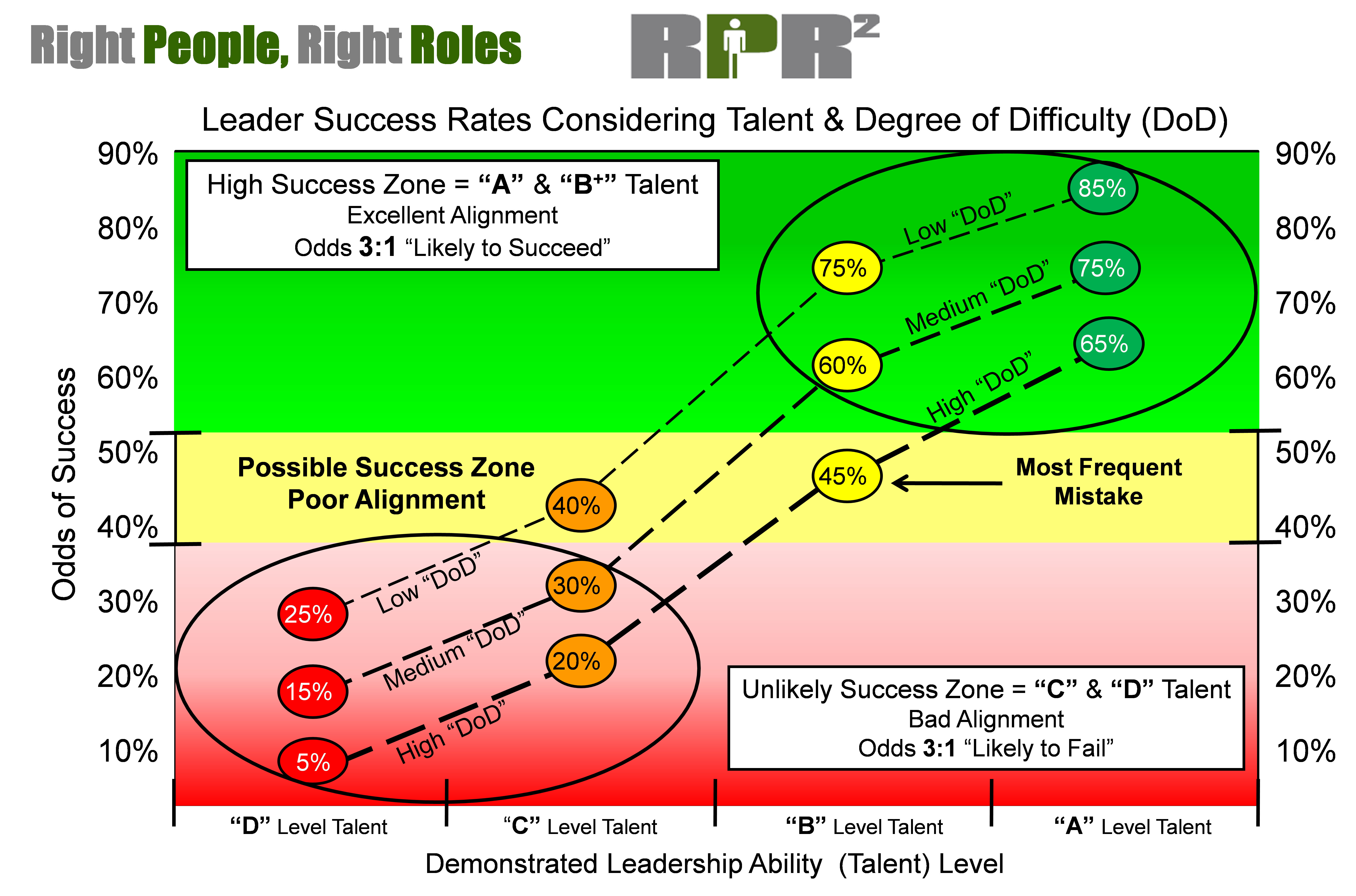
Figure 5. Leader Success Rates Considering Talent & Degree of Difficulty. This figure represents odds of success for A, B, C and D level talent based on degree of difficulty of their role.
7. Coach early and often. Don't wait until someone is struggling or failing before intervening. At that point, coaching intervention will not work. It's not fair to use the coaching process as a "Hail Mary Pass." Coaching is not remedial. It is for the truly effective leaders and those dedicated to its pursuit.
8. Accelerate performance improvements that drive out waste and compound productivity. Implement a structured approach to reduce or eliminate unnecessary procedures, steps within processes and total numbers of people involved to make decisions. This management competency is essential to achieve long term financial success.
9. Create acceptable protocol for management meetings that allows for the right people to attend the right meetings rather than the current out of control state where there are too many unnecessary people attending too many unnecessary and inefficient meetings.
10. Separate the "Signal from the Noise." Create an acceptable protocol for e-mail messages. Copy the right people at the right levels of communication so e-mail volume is manageable. E-mail may be a technologically efficient way to communicate, but it is a very ineffective way to conduct a compelling conversation.
11. Push management decisions down vs. requiring permission by senior executives to make basic day-to-day decisions. The current environment of "seeking approval" from executives has reached the management equivalent of requiring "sign-off" financial responsibility for expenditures of $10.00 or more! Grant front-line managers autonomy to make day-to-day decisions.
12. "What gets you here, won't get you there." Marshall Goldsmith's best-selling business book says it all. Success at the next level of leadership responsibility requires different skills and often a different mind-set perspective. Lack of self-awareness, limited emotional intelligence, limited skills or sense of position entitlement can significantly impact performance at advancing levels of management responsibility.
These facts and the longitudinal trends we have measured since 2004 inspired this list of insights, observations and possible solutions to the unintentional acceleration of the Peter Principle in healthcare. Consider how your organization will adjust business practices to get the right people in the right roles.
Tom Olivo, CMC, is the founding partner in the consulting firm Healthcare Performance Solutions and the president of Success Profiles, Inc. Established in 1990, Success Profiles designs and provides organizational performance measurement instruments and database management services to clients, management consulting firms and professional associations. In his professional career, Mr. Olivo has over 25 years of experience in identifying, measuring and comparing the "commonalities" of highly successful athletes, business leaders and organizations.
James Jiloty, M.S., PHR, has spent his entire career in the healthcare industry since 2003, with expertise in human resources development and leadership. He is a valued business partner to clients engaged in a structured approach to talent development and performance improvement strategy.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker's Hospital Review/Becker's Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.


