The annual budget process provides a unique opportunity for finance leaders to identify savings for the upcoming fiscal year.
According to the American Hospital Association, labor costs account for almost 60 percent of all healthcare costs and are the biggest factor in the growth in hospital costs across the country. Since CFOs have a critical role in making healthcare more affordable, managing labor costs should be a key area of focus in the annual budget process.
In years past, CFOs squeezed out labor costs through incremental improvements, but the remaining savings on labor costs will come from re-envisioning our view of managing labor costs in the budget process.
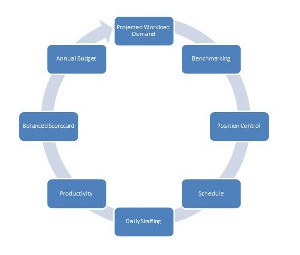
Let us begin then to understand how we can develop a cycle to continuously improve labor expenses and refine the budget process to find additional savings.
Patient flight path generates demand
First, an organization should start by collecting information on the flight path of the patient. By understanding the flow of patients, an organization can then project workload demand for every department. This workload projection will vary by service line. For example, the organization could measure visits to the clinic, average daily census in the hospital, square footage or other metrics.
With projected workload demand, staffing standards can be developed based on industry benchmarks. These benchmarks could either be based on publicly reported data, for example many hospitals in California report staffing levels to the Office of Statewide Health Planning and Development. Or, a number of vendors, such as Truven Analytics, compile benchmarking information across the industry. Staffing standards should be refined and agreed to jointly between finance and operations and may need to be adjusted for changes in market requirements, local regulations or other operational needs.
A position control tool for the future
With information on the workload demand and staffing standards, an organization can then develop a "position control" tool. The tool will help inform everyone from the C-suite to frontline hiring managers on their hired FTEs compared with their required FTEs based on the workload demand and staffing standards. A strong position control tool will not only help guide the budget process but also will help frontline managers manage their payroll expense as the fiscal year unfolds.
The other benefit of this approach is your payroll budget and hiring plans can be scaled up or down when you have a change in workload demand. For example, if an ICU manager has twice the number of admitted patients than expected, it would not be reasonable for them to meet their payroll budget, and their hiring plans should adjust accordingly.
Translating a hiring plan into daily operations
In operational departments, the position control translates into a master schedule, which is the core driver of hospital expenses. Hospitals should keep a close eye on the staffing schedule posted on the wall at it is the largest driver of hospital expenses.
The schedule translates into daily staffing, which accounts for fluctuations in demand, sick calls, acuity of patients and more. By leveraging the learnings from the workload projections collected in the first step, you can be prepared for every scenario. For example, organizations can utilize current clinic visits to project out future labor and delivery visits by month.
Monitoring performance
Even the best-laid plans in the budget process will need to evolve as the market changes. With that in mind, hospitals can use labor productivity tools to monitor daily staffing performance. And while CFOs have a fiscal responsibility, this should not come at the expense of quality and service. Therefore, a balanced scorecard that weighs quality, service and financial performance is critical to monitor adherence to the budget and operating plans.
Performance improvement in the budget process
CFOs are well versed these days in identifying opportunities and driving change using performance improvement principles. But how many CFOs apply those same principles to the budget process itself? With that in mind, CFOs and senior leaders should leverage performance improvement principles to eliminate waste and streamline the budget process. Frequently, wasted time and effort in the budget process distracts from a CFO’s ultimate objective of driving affordability.
 A multi-year approach
A multi-year approach
As finance leaders, we should now consider the annual budget as part of a multi-year financial and workforce planning strategy with the budget as a critical tool in realizing this multi-year vision. CFOs cannot treat the budget as their sole opportunity to impact costs, and many levers require more than 12 months to realize. Opportunities for savings are now frequently found in more complex processes spanning across multiple departments. Therefore, the solutions required have become more complex and take longer to realize.
The budget process as an engagement opportunity
As a finance leader, the budget process is a key moment to engage your staff. The process should be about more than numbers — it is an opportunity to gain supporters for your vision and financial strategy. Many CFOs have a tendency to be cynical of department leaders during the budget, but I think Ken Blanchard, author of "The One Minute Manager" said it best: "None of us is as smart as all of us."
In conclusion, the best approach for CFOs to improve affordability and find savings in the budget process is to understand the demands of the patient and provide meaningful targets to operational leaders using benchmarks. CFOs should provide a vision for the future, and crystalize the focus on the important elements in the budget. Then, get out of the way and realize that the best solutions will most likely come from those around you.
Christopher "Chip" Neuman, is area finance officer at Kaiser Permanente and is completing the Executive Masters in Healthcare Leadership program at Brown University in Providence, R.I.

