Healthcare is undergoing a shift from a fee-for-service to a value-based services paradigm due to the new reform efforts being adopted at a national level. In the United States, the transition in payment models is a result of what is quickly becoming a bankrupt healthcare system and the need for change with an aging population.
As a result, clinical leaders find themselves in an environment of increasing financial pressure, legislative mandates and dwindling reimbursement. All of these factors contribute to a stream that is increasingly running dry for many organizations. Healthcare organizations face the new complexity and reality of managing assigned patient populations within a defined catchment area. Population health and wellness is the new mantra, rather than a reimbursement model based upon disease and illness.
What is population health management?
Understanding how to manage patients within a population health model is the new core competency for leaders who want to remain viable and agile within the newly emerging healthcare landscape. Under value-based contracting where incentives are tied to outcomes, different healthcare sectors are joining forces to provide services in the most appropriate setting, efficiently and economically, while still maintaining the level of care patients need. The hospital emergency department becomes a portal of last resort and preventative health becomes the key to maintaining a patient's health and quality of life.
Population health management is an approach that seeks to maximize a defined population's health, while at the same time minimizing expenses. This includes preventing costly interventions such as emergency department visits, hospitalizations, imaging tests and procedures 1. The Institute for Health Technology Transformation 2 formally expanded the definition for greater clarity to note that population health management conceptually, "…not only lowers costs, but also redefines healthcare as an activity that encompasses far more than sick care. While [population health management] focuses partly on the high-risk patients who generate the majority of health costs, it systematically addresses the preventive and chronic care needs of every patient. Because the distribution of health risks changes over time, the objective is to modify the factors that make people sick or exacerbate their illnesses."
From a continuum of care perspective, population health management involves a greater reliance on community resources for individuals, access to education programs about wellness and self-actualization for individuals who want to engage in healthy lifestyles through behavioral changes. More cohesive communication is necessary in the newly emerging models to ensure continuity of care as patients transition over what could historically be called gaps in their care (the hospital to home, specialist to primary care physician, primary care physician and the provision of in-home services). Federal and state programs and policies, such as the Health Information Technology for Economic and Clinical Health Act, meaningful use, and health information exchanges have been enacted to help support a hospital and clinician's ability to establish the necessary information technology infrastructure for cohesive communication. Population health management is increasingly viewed as the solution to the growing financial pressures of an aging demographic, legislative mandates to improve quality at lower costs and reimbursement taking on financial (dis)incentive structures.
Why transitioning to a population health focus is important
Many of the emerging coordinated care infrastructures embrace a population health perspective as a requisite. Accountable care organizations are required to track and monitor the risk level of their population assigned by CMS 3. Taking a proactive approach to wellness is common sense — but organizations need to stratify the healthy from those who will need health services or incur substantial costs. Statistical averages of population health are no longer adequate; stratification must now occur at the individual level. Through health risk assessment and tracking trends, organizations have a way to reduce costs and specifically target individuals to promotion self-care. The 'population' becomes more manageable when efforts can be spent wisely on the individuals who are projected to cost the most.
For self-insured health systems and medical groups, the employer assumes the financial risk for services provided to the population pool (their employees). Under a self-insured arrangement, the insurance carrier and premiums are removed from the process because the employer bears the full responsibility of the claims as they are incurred. The self-insured organizations function much like ACOs. When high claim volumes or expenditures accrue, it is the organization that becomes at-risk. Risk stratification then becomes not only necessary but also a tool for viability.
Through contracting, payers are quickly aligning with shared savings programs. The goal of these arrangements is analogous to the self-insured groups and ACOs. Money remaining in the coffers at the end of a year is split between the payer and the partnering organization. Under these value-based service contracts, providing efficient and cost-effective care while keeping claims to a minimum serve as a sharp contrast to the fee-for-service model.
There is also a heightened focus on Medicare Advantage patients to create healthier lifestyles and mitigate health risks. The Patient Protection and Affordable Care Act included a provisionallowing Medicare beneficiaries to receive an annual wellness exam. A portion of the exam includes a health risk assessment for better management of the patient's conditions and an individualized approach to patient education.
Connection to the IHI Triple Aim Model
The Institute for Healthcare Improvement developed the Triple Aim Model as a way to optimize health system performance. The Triple Aim components include: Improving the patient experience of care (including quality and satisfaction), improving the health of populations and reducing the per capita costs of healthcare 4. Defining patient populations that are at-risk for health decline fully aligns with the Triple Aim. Education that is individualized to the patient has been shown to improve patient satisfaction and the ability to self-manage conditions 5 6. Converting patients to focus on maintaining the highest level of health possible, rather than an episodic treatment approach, combined with individualized education of their risk factors, is an effective method of providing patient-centered care.
The illness to wellness conversion: predictive scales being used
There are different scales that can be used as part of a wellness plan to identify risk. Validated measures provide the statistical security of knowing the scale accurately predicts health outcomes as designed. Each of the scales is an independent assessment of an individual.
1. Probability of repeated admissions scale. The PRA scale is a validated, predictive measure for individuals aged 65 and older, which determines a patient's risk for multiple hospitalizations. Scores are based upon weighted factors by a respondent including self-reported health status, age, gender, prior hospitalization and ambulatory visits, presence of a caregiver and diabetes or a coronary condition either reported or under medical treatment 7.
2. Frailty scale. The frailty scale is also a validated, predictive measure for individuals aged 65 and older. It examines the individual's likelihood of requiring nursing home or long-term care within a two-year window. Scores are based upon weighted factors by a respondent, which include age, assistance with medications, bathing and interference with activities of daily living 8.
3. Depression Scale. The depression scale is an identification tool, rather than a diagnostic tool, that identifies a need for a behavioral health evaluation. It uses the Patient Health Questionnaire-2 series of questions on a zero to three point scale. The total number of points identifies the need for further clinical evaluation to rule out a depressive disorder. Depending upon the probability, either a further assessment or an interview may be indicated 9 .
4. Predicted insurance expenditures scale. The PIE scale is a predictive measure that determines which individuals between the ages of 18 to 64 are most at-risk within the next 12 months for above-average health care expenses. The scale includes the respondent's age, gender, use of medications, volume of needed prescriptions, number of prior physician visits and self-reporting of diabetes, arthritis, high cholesterol or a history of cancer 10.
Through use of the various validated scales, clinicians can focus on wellness and preventive care solutions for patients who need intervention the most. Those most at-risk for a condition can be identified through predictive measures that help the healthcare provider better assess and direct the individual's health needs prior to requiring services.
Types of health risk assessments being adopted in the industry
Depending on an organization's level of maturation with assessing health risk of their defined population, one of four types of health risk assessments is being used to determine those individuals that need additional focus (see graphic 1). These four types include a demographic risk and propensity model, demographic wellness program and individualized health risk assessments and wellness programs. Identifying where your organization falls within the four types can help leaders understand where they presently reside in their level of maturation and the level they desire to achieve for their target population.
Having a basic population health awareness of your membership as a whole is the entry level for a wellness program. The upper left quadrant seeks to identify what you know about your population as a whole.
The second level of maturation is adopting a risk and propensity model. The lower left quadrant is for organizations that break their total population into subgroupings, such as risk according to chronic conditions. This category of wellness programs also seeks to identify which members are engaging in some level of preventive health. Messaging can be individualized and targeted to specific populations, such as patients who have chronic heart disease.
The third level of maturation is conducting individualized health risk analyses. The quadrant in the upper right moves beyond categories of populations to the individualized member or patient. The organization has shifted from generalized programming to validated risk measures for understanding their population.
Once organizations or payers have migrated from an overall population view to an individualized member view for understanding an assigned population's health status, it becomes easy to shift to the fourth and highest level of wellness program maturation in the lower right quadrant. Stratification of the membership enables organizations to undertake individualized wellness program outreach on a manageable scale. Member-specific wellness programs go beyond the one-size-fits-all approach and tailor wellness plans according to knowledge of specific members. Individuals within a population have different health risks. Accordingly, the wellness plan has matured to implement programming that is tailored to high-risk individuals on a per-person level of focus. This level of wellness program has the greatest ability to produce a ROI for an organization or payer because of its granularity and the proven success of working with assigned members on an individualized level. Program outcomes can be tracked over time, not only for the overall program, but also for each individual.
Graphic 1. Levels of health risk assessment maturity.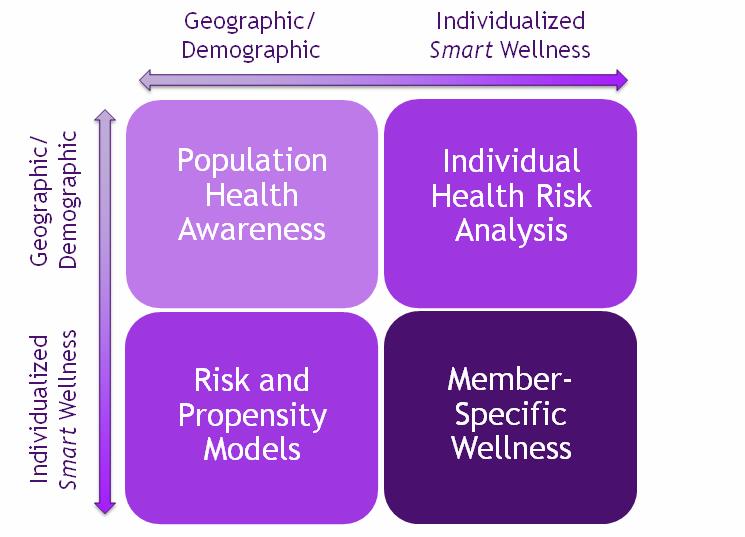
Wellness Program Evaluation
After an organization determines the level of wellness program they want for their members to identify those that are most at-risk for services utilization, the next step is to provide program transparency within the organization. The program visibility helps to identify improvements that can be made, both at an organizational and individualized member level, for providing outreach. This often involves a care coordination team or nurses who work with high-risk individuals.
One benefit of providing a wellness program to members with health risk assessments is the additional capability to trend outcomes over time. As the top tier of individuals who incur claims becomes monitored and focused on for health improvements, the patients in that tier shift to lower levels of risk. Repeated measurements of the population enable an organization or payer to see the progress being made through program outreach, in addition to the reduction in claims and improved quality of life for individuals within the program.
As with any type of program adoption, sustainability is the key to success. When metrics and tracking become part of the program, the likelihood of sustainability is increased through the dedicated focus, transparency and ability to see changes over time. Two layers of sustainability are important within a risk assessment program. The first is the organization or payer's ability to continually improve outcomes for their assigned population. The second layer of sustainability is at the individual level, where those within the population want to achieve a state of better health or maintain a level of wellness without further deterioration. To assess this level within an individual, the Patient Activation Measure scale is a valid and reliable tool that is used to determine an individual's level of self-actualization.
The PAM scale has four stages, which involve the individual believing their role is important, having the ability and knowledge necessary for action, taking action and sustaining change 11 . Knowing where an individual resides within the four levels helps clinicians create individualized interventions and assess actualization changes to modify care plans. Scoring ranges between 0 to 100, which provides insights into attitudes, motivators, behaviors, and outcomes. Through patient engagement, individuals become more likely to adopt necessary changes and remain compliant with their treatment plans or desired behaviors 12 13. Additionally, an individual's PAM score can be monitored over time as a key indicator of self-actualization and ability to engage in behavior change as a component of wellness program adoption.
As leaders seek to find ways to control costs through a population health approach and value-based services paradigm, understanding a population and high-risk constituents becomes important. Using validated measures to gain insights about a population helps to provide reliable information so payers and organizations can partner with patients and consumers for better health. When patients are involved in their own care, the willingness to remain compliant with a treatment plan increases. Similarly, using a preventive health model, organizations and payers need to reach individuals even before they access the healthcare system. Understanding the different evolutionary stages of wellness programs, and where your own organization fits within the four-quadrant level of maturation, is the first step toward providing care that resonates with individuals and establishes ROI within a shifted focus from illness to wellness.
Jennifer Volland is vice president of program development at National Research Corporation where she has oversight of program development for many of the company's service lines. She regularly speaks as a faculty presenter with The Governance Institute on quality and improvement methods to drive organizational outcomes. Jen has a bachelor's degree in psychology and an executive MBA from the University of Nebraska at Omaha, a bachelor of nursing from Creighton University and is in final candidacy for a doctor of health administration degree from Central Michigan University. She is triple board certified and is involved in national certification exam development with the American College of Healthcare Executives and the American Nurses Credentialing Center.
1 Lisk-Felt, S., & Higgins, T., (2011). Exploring the promise of population health management programs to improve health. Mathematica Policy Research Issue Brief. Retrieved from http://www.mathematica-mpr.com/publications/pdfs/health/PHM_brief.pdf.
2Institute for Health Technology Transformation, (2012). Population health management: A roadmap for provider-based automation in a new era of healthcare. Retrieved from http://ihealthtran.com/pdf/PHMReport.pdf
3 CMS Fact Sheet (2012). Summary of final rule provisions for Accountable Care Organizations under the Medicare shared savings program. Retrieved from http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/ACO_Summary_Factsheet_ICN907404.pdf
4 IHI (2013). The IHI triple aim. Retrieved from http://www.ihi.org/offerings/Initiatives/TripleAIM/Pages/default.aspx
5 Hillen, J. S., Beaton, S., Fernandes, O., Von Worley, A., Benitez, G. V., Hanson, A… (2013). Are benefits from diabetes self-management education sustained? American Journal of Managed Care, 19, 104-112.
6 Oliver, J. W., Kravitz, R. L., Kaplan, S. H., & Meyers, F. J. (2001). Individualized patient education and coaching to improve pain control among cancer outpatients. Journal of Clinical Oncology, 19, 2206-2212.7 Pacala, J. T., Boult, C. & Boult, L. (1995). Predictive validity of a questionnaire that identifies older persons at risk for hospital admission. Journal of the American Geriatrics Society, 43, 374-377.
8 Brody, K. K., Johnson, R. E., & Ried, L. D. (1997). Evaluation of a self-report screening instrument to predict frailty outcomes in aging populations. The Gerontologist, 37, 182-191.
9 Kroenke, K., Spitzer, R. L., & Williams, J. B. (2003). The patient health questionnaire-2: Validity of a two-item depression screener. Medical Care, 41, 1284-1292.
10 Boult, C., Kessler, J., Urdangarin, C., Boult, L., & Yedidia, P. (2004). Identifying workers at risk for high health care expenditures: A short questionnaire. Disease Management, 7, 124-135.
11 Hibbard, J. H., Stockard, J., Mahoney, E. R., & Tusler, M. (2004). Development of the Patient Activation Measure (PAM): Conceptualizing and measuring activation in patients and consumers. Health Services Research, 39, 1005-1026.
12 Cooper, L. A., Roter, D. L., Carson, K.A., Bone, L. R., Larson, S. M…(2011). A randomized trial to improve patient-centered care and hypertension control in underserved primary care patients. Journal of General Internal Medicine, 26, 1297-1304.
13 Newell, D., & MChiro, R. B., (2012). Increasing compliance toward home exercise in chiropractic patients using SMS texting: A pilot study. Clinical Chiropractic, 15, 107-111.
More Articles on Population Health Management:
3 Challenges to Integrating Population Health Into Healthcare
Paying for Population Health: Why Rewarding Value is Key
Taking a Patient-Centered Approach to Population Health Management

