On March 14, 2014, CMS issued guidance "Requirements for Hospital Medication Administration, Particularly Intravenous (IV) Medications and Post-Operative Care of Patients Receiving IV Opioids."
This guidance recommends "at a minimum" [page 19] that hospitals "have adequate provisions for immediate post-operative care, to emphasize the need for post-operative monitoring of patients receiving IV opioid medications, regardless of where they are in the hospital." [page 1]
In addition and more importantly, the CMS guidance necessitates monitoring for all patients receiving opioids when in hospital:
"Narcotic medications, such as opioids, are often used to control pain but also have a sedating effect. Patients can become overly sedated and suffer respiratory depression or arrest, which can be fatal. Timely assessment and appropriate monitoring is essential in all hospital settings in which opioids are administered, to permit intervention to counteract respiratory depression should it occur." [page 15]
What does the CMS guidance mean by "appropriate monitoring"?
Does "appropriate monitoring" mean intermittent assessment, as was recommended in last year's CMS proposed quality measure (#3040)?
Proposed measure #3040 provided that monitoring needs to be "documented" and the time between documentation must "not exceed 2.5 hours." This means that a nurse or other caregiver must document the patient’s condition and do this in intervals of not greater than 2.5 hours.
In the report submitted after the CMS guidance was released by the National Quality Forum to HHS, the measure was not endorsed and it was decided that the measure "requires modification or further development."
Robert Stoelting, MD, president of the Anesthesia Patient Safety Foundation, in commenting on proposed measure #3040 said:
"The conclusions and recommendations of APSF are that intermittent 'spot checks' of oxygenation (pulse oximetry) and ventilation (nursing assessment) are not adequate for reliably recognizing clinically significant evolving drug-induced respiratory depression in the postoperative period. For the CMS measure to better ensure patient safety, APSF recommends that monitoring be continuous and not intermittent, and that continuous electronic monitoring with both pulse oximetry for oxygenation and capnography for the adequacy of ventilation be considered for all patients."
Or does "appropriate monitoring" mean continuous electronic monitoring?
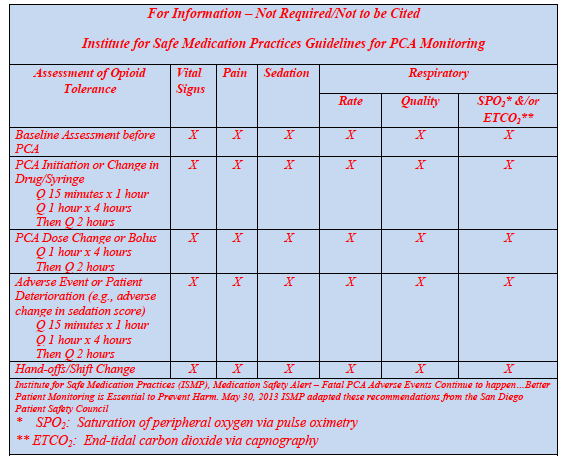
The CMS guidance provides two examples — one from the Institute for Safe Medication Practices and one from APSF — which could suggest that the guidance may be referring to continuous electronic monitoring. For example, the guidance provides the following from ISMP which refers to monitoring for saturation of peripheral oxygen via pulse oximetry and end-tidal dioxide via capnography:
The CMS guidance also refers to APSF recommendations (see below) and its recent video on opioid-induced ventilatory impairment.
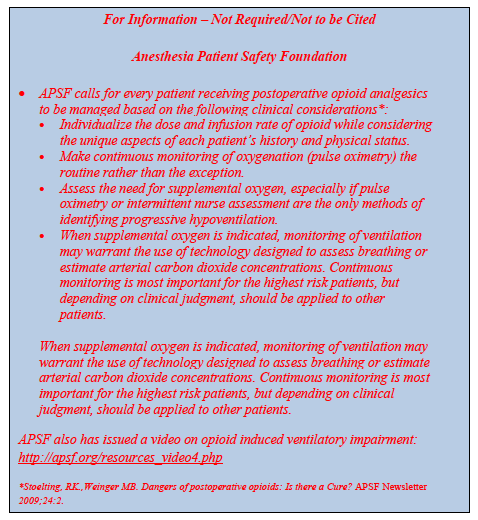
In its video, APSF states that continuous electronic monitoring of oxygenation and ventilation, when combined with traditional nursing assessment and vigilance, will greatly decrease the likelihood of unrecognized, life threatening, opioid induced respiratory impairment. The clinical significance continuous electronic monitoring offers is the opportunity for prompt and predictable improvement in patient safety.
APSF is calling for a paradigm shift in opioid safety. According to APSF's Dr. Stoelting:
"It's time for a change in how we monitor postoperative patients receiving opioids. We need a complete paradigm shift in how we approach safer care for postoperative patients receiving opioids."
Could CMS guidance have saved a life?
Following this CMS guidance for monitoring of patients receiving opioids wherever they are in the hospital could have saved the life of 18-year old, Amanda Abbiehl.
Amanda was admitted to hospital for severe step throat. She did not receive surgery. She was placed patient-controlled analgesia to manage her pain, but was not monitored.
As Amanda's father asks:
"It isn't standard practice to monitor patients with Capnography. However, if Amanda’s CO2 level had been monitored, wouldn’t this have alerted her caregivers so her life could have been saved?"
By this measure — continuous electronic monitoring with traditional nursing assessment and vigilance — Amanda may still be alive today. For this, CMS should be applauded for its new guidance.

