Since the Patient Protection and Affordable Care Act of 2010 – commonly referred to as the ACA, hospitals and other healthcare facilities have been determined to meet the new standards of quality built into the law, and mitigate the risks associated with the negative incentives associated with the law's enforcement.
The Centers for Medicare and Medicaid's Fiscal Year 2014 Inpatient Prospective Payment Systems final rule, going into effect FY 2015, expanded applicable conditions for readmissions measures to include Chronic Obstructive Pulmonary Disease exacerbations - COPD is the third leading cause of death in America and is responsible for over 700,000 hospitalizations and 1.5 million emergency department visits every year.
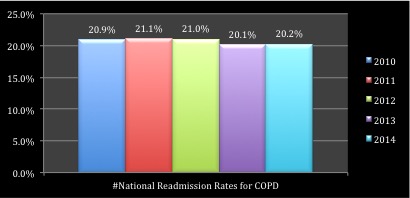
Readmission rates for COPD are stable
Although 30-day all-cause readmission rates are decreasing, COPD rates remain stable, above the CMS benchmark at 20.2%. Not only are the national 30-day readmission rates for COPD remaining high, the nation's "Top 15 Health Systems" have not made significant progress towards reducing this discrete number, although they are lower than the national average at 19.9%.
Hear are 5 things to know about utilizing local ancillary providers to manage your hospital's post-acute care COPD patient population to reduce readmissions.
1. Ancillary providers are making headway
There is a distinct network of ancillary providers that have been contracted by hospitals to provide post-acute transitional care for their COPD patients. 30-day COPD readmission rates among this network of providers is 65% less than the "Top 15 Health Systems" and 67% less than the national average. This network of ancillary providers has a mean COPD readmission rate of 6.9% among this patient population.
For example, Life HME, an ancillary provider located in South Carolina has an established post-acute care transition program for patients. Along with nurses, health coaches and respiratory therapists to follow patients, they have integrated a cloud-based care coordination platform that enables the multidisciplinary team to communicate and track patient progress post discharge. Dewey Roof, President of Life HME briefly describes the marriage between homecare and technology, "Our care specialists act as an extension of the hospital's care team by enabling discharge planners to schedule and track patient care in real-time through our platform [HealthCall]."
It's hard to argue that this collaboration hasn't made a dent in COPD readmission rates. Since its first patient, using the HealthCall cloud-based platform, Life HME has a 15.8% readmission rate with its patients; in 2015 this rate has dropped to 13.64%.
2. Ancillary providers are already integrated into the care of the patient
Most post-acute patients are aligned with a nurse-directed disease management program that focuses on controlling exacerbations through ongoing assessments and monitoring, pharmaceutical management and reducing risk factors. Many of these programs also utilize the expertise of registered Respiratory Therapists that are employed through a contracted or hospital-owned durable medical equipment company. Although RRT's are not typically employed to monitor patients, they are already involved in the post-acute care of the patient, utilized primarily to deliver and educate patients on the use of oxygen and related equipment in their homes.
3. Ancillary providers have capacity as hospitals become leaner
As hospitals transition from volume to value incentives, price pressures and pay for value formulas are forcing hospitals to reduce operating costs and reduce costs per episode of care. These pressures are placing a laser focus on staff capacity and new position creation.
Many independent ancillary providers have additional capacity, or can easily flex up, to be an integral part of the post-discharge care plan; it is reasonable to suggest this capacity is limited within the hospital ancillary providers, as lean and six-sigma processes have increased in popularity.
4. Ancillary providers offer a lower cost solution to transitional care
Many of the alternatives for transitional care can be expensive unless the hospital has nursing staff or ancillary providers with capacity to handle the operations of a program. Many alternatives utilize call centers, medical devices and "high-end" human resources (physicians and extenders, nurses) to manage care plans and patient algorithms.
Ancillary providers manage the patients in the normal course of their daily activities, which adds minimal costs to the hospital contracting with the service. Ancillary providers also have the nimbleness to adopt and integrate less expensive technologies, where large hospital systems can move much more slowly in adopting new technologies due to multiple-stakeholder buy-in.
Many of these ancillary providers are willing to work with hospitals on a shared-risk basis. This enables hospitals to lower financial risks in contracting with these providers to reduce sizeable penalties for exceeding CMS standards, as well, it incentivizes ancillary providers by sharing rewards for readmission reductions.
5. Innovative technology use
Technological advances in communications have been developed that decrease the human resources needed to manage chronic populations. Cloud-based communications are cheaper than implementing more traditional electronic medical record platforms to accommodate the communication needs to follow patients. Automated patient engagement systems also replace high-cost call centers, as well are directly integrated with the EMR to create a seam "less" environment for all providers to be up-to-date on the health of their managed population.
At Life HME, Mr. Roof is excited about other quality metrics the platform allows his company to track. He was quick to tell us about how many patients adhere to the program's care plan. "We can track through automated assessments the percentage of patients adhering to our plan of care. The national average is 21% and we are seeing a 72% adherence. This is exciting for us as this means what we are doing is effective in engaging patients in their own health."
Author's Bio:
Kent has spent 26 years in healthcare, with the last 15 years focused on administration in for-profit and not-for-profit companies in the mid-west. Currently he is the managing principal of BusinessPsycle, LLC, a consulting collective focused on sustainability business models, quality analytics, strategic planning and resource stewardship. Kent earned a master's in business administration from the University of Notre Dame and is working on his PhD in Organizational Psychology – focused primarily on behavioral economics.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker's Hospital Review/Becker's Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.

