Whether it be through the formation of an accountable care organization, taking capitated or risk-sharing reimbursement or simply wanting to build a better model for patient care, health systems require new capabilities to operate successfully in a population health environment.
As part of Health System Advisors' research on remaining relevant in a rapidly changing environment, we've outlined four capabilities health systems must develop in population health.
Building Population Health Capabilities
Managing a population's health requires dramatically different capabilities than delivering care to sick populations. As such, health systems wanting to take on population health reimbursement risk must rapidly acquire and/or build a new set of capabilities. National research in building an ACO and managing population health risk has shown there are four capabilities critical for health systems to develop, including:
1. Capability to define and adapt the care model based on the unique populations' needs
2. Capability to identify, collect, analyze, and report health information about the managed populations
3. Capability to manage the patients' navigation through a clinically appropriate care process
4. Capability to build and manage a broad network of continuum partners
The health system's success in creating these capabilities is a key indicator for its future population health success. While these capabilities can be rented or bought in the short term, if they are not developed inside the organization, long-term success will be limited.
1. Defined Care Model
A care model that represents comprehensive service delivery by integrating data analytics, best practices with providers, and care teams at the point-of-care, via administrative infrastructure (CMOs/executives/finance oversight) and decision support is the requirement in today's marketplace. The care model almost always has three overarching goals:
1. Improve clinical outcomes
2. Reduce the overall cost of care
3. Improve patient satisfaction
To acheive these goals, the care model must:
- Shift high-risk patients from high-cost care to primary care physicians and care team management evidenced by improved disease management measures, self-rated health and engagement in care, in addition to reduced hospitalizations, emergency room visits and avoidable readmissions.
- Move moderate-risk patients from costly episodic care and avoid movement into the high-risk category to becoming self-sufficient in the management of their care.
- Maintain a healthy status in those patients identified as low-risk evidenced by pairing with a PCP, participation in preventive screenings and avoiding unnecessary hospitalizations and emergency department visits.
For most care model designs, integrating providers, is often the most effective way to engage patients and impact spending. The design of this integrated provider-based care model must:
- Scale the solution to employers outside the traditional health system markets;
- Benefit patients and payers through development of a network dedicated to improving quality and managing care;
- Provide incentives and/or ties provider compensation to performance scorecards;
- Quality based requirements (process and outcome measures)
- Provider level utilization data
i. Support network-wide standard clinical protocols;
ii. Allow for multi-member contracting under single entity; and
- Build scalable infrastructure to support population health management across multiple populations.
2. Health Information Support
A robust, central infrastructure is necessary to build a scalable platform for population health management. There are common elements the information system must have, including:
- Centralized data warehouse with data mining capabilities
- Automated tools to support closing care gaps
- Clinical quality and utilization metrics, specific to providers
- Report building, including total cost of care elements for each employer across populations
- Care navigation support tools
- "Bolt-on" tools for clinical decision support
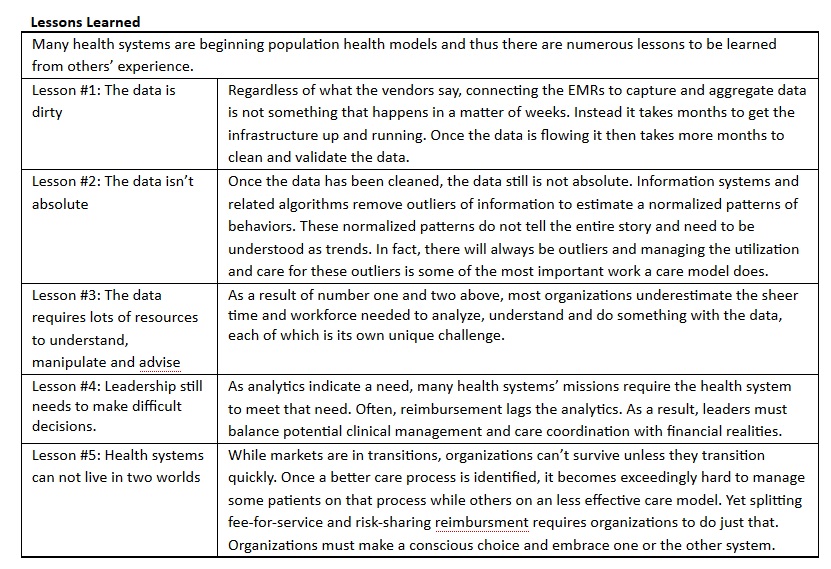
Today, no single information system addresses all the information needs of the typical health system. As a result, when building its population health infrastructure, health systems must consider which information system gaps are easier to fill or less important for their success. Often health systems will focus on leveraging their EMR capabilities. There are two important considerations when vetting this option. First, EMRs are fundamentally episodic documentation tools, not designed to provide population management capabilities. Second, depending on the network configuration, independent providers or affiliated providers on varying EMRs present a barrier to complete integration when utilizing the health system's EMR-based solution.
Our experience with the data flowing in from various systems shows significant validation is required. This is always underappreciated in the timelines and implementation process. However, the more effort put in up-front, the more acceptable the data will be to the end-users. Often this validation process can be partially outsourced, but the ongoing need for report generation and follow up analysis will necessitate building an internal Business Intelligence Team. The scale of this team will be far more than the vendors suggest. It is reasonable to assume that an initial team may be made up of a director of business intelligence and one to two analysts. As reports begin to be generated, the number of business intelligence team members may easily grow to 10 to 12 full-time equivalents within the first two years for a moderately sized risk contract.
3. Care Navigation/Management
The purpose of care navigation is to pair data and proven care models to improve the populations' health. A tried and true way to deploy the care navigation models is to focus on areas of the greatest need.
Industry based analytics illustrate that 3 to 5 percent of a population accounts for driving 50 percent of a commercial population's total healthcare spending. Utilizing data to support varying degrees of intervention and support for high risk, high cost persons can make a large impact. Deploying a care navigation model, integrated within the Patient Centered Medical Home, supports appropriate care navigator intervention on high-risk patients. Further, care navigators can also monitor the low- and moderate-risk patients for selected leading indicators to identify cases for early intervention.
4. Network of Partners
Successful contracting requires presenting the market with a broadly accessible and complete specialty network. Typically, the initial network will begin with health system-employed and traditionally aligned, independent providers. Using this hospital-centric approach will leave coverage gaps. These gaps are typically found in specialties that do not admitt to the hospital or in areas downstream from the inpatient admission. Filling these coverage gaps requires the health system to use relationship skills to create community partnerships covering the care continuum.
Managing the partners requires different tools. Whereas providers in the clinically integrated network will have influence in defining their care management role, the sheer numbers of providers limit the dependence on individual providers. However in some continum partnerships, there may only be a handful of contracted organizations providing the service (e.g., home health, SNFs, etc.) thus raising the importance of individual organizations' partnerships and performance.
Building this network in a clinically integrated provider model is most efficient. Approaching the market as a single-signature organization creates both leverage with and efficiency for the payers and direct to employer negotiations. As a result, nearly all long-term risk-taking organizations are organized around a clinically integrated model.
Kate Lovrien and Luke C. Peterson are principals at Health System Advisors. They have more than 30 combined years advising senior healthcare leaders on their market and organizational strategy. They can be contacted at Kate.Lovrien@HealthSystemAdvisors.com or Luke.Peterson@HealthSystemAdvisors.com.
Health System Advisors is a strategy consultancy focused on advising leaders, advancing organizations, and transforming the healthcare industry. www.HealthSystemAdvisors.com.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker's Hospital Review/Becker's Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.


