The recent political turmoil around health reform highlights an unfortunate reality – health policy in the United States is not driven by clearly defined, consensus-driven goals and measurable outcomes.
The approach taken by lawmakers continues to lack a basic performance measurement framework. In particular, there are no specific performance targets that account for the inherent trade-offs, and there is virtually no way to make timely and meaningful corrective actions when problems are identified in the system. This two-part series will focus on how addressing these basic issues could help set the US health and health insurance industries on a sustainable path.
Specific Targets, not Platitudes
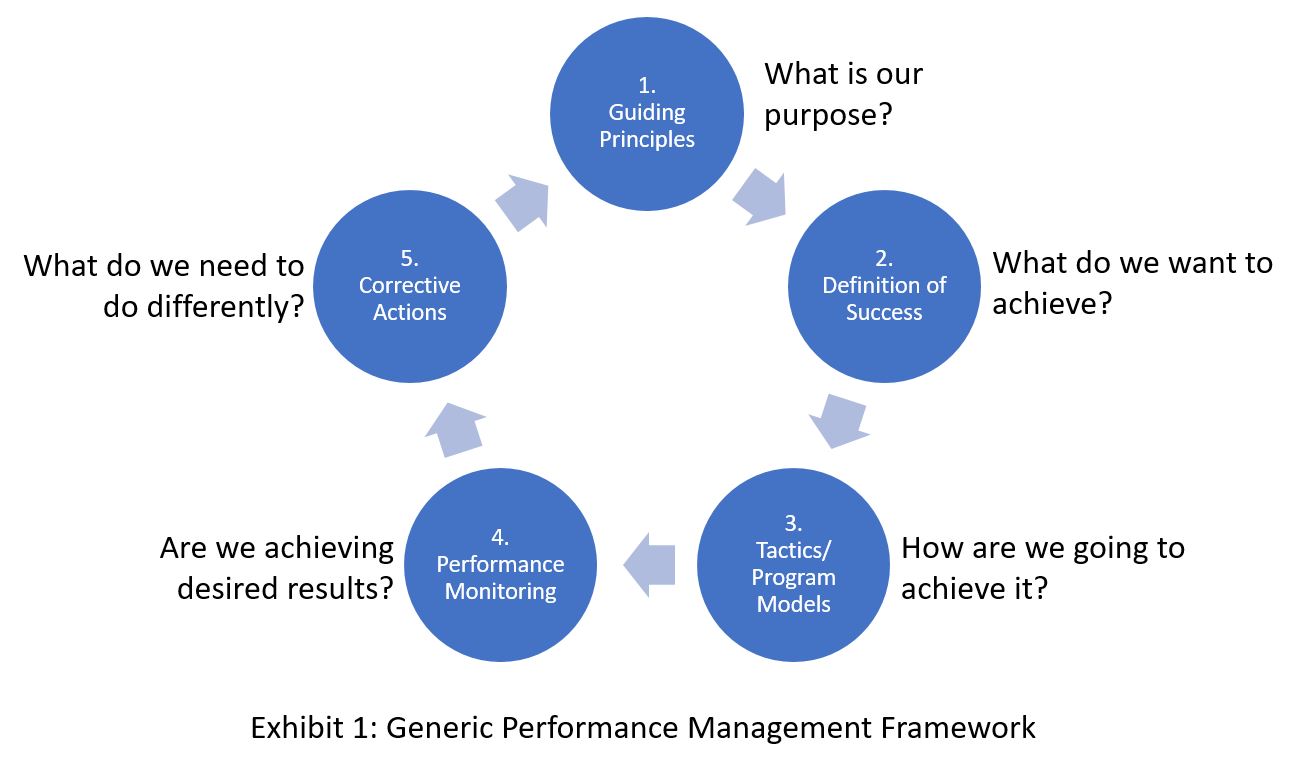
Both major political parties in the US actually seem to agree on the purpose of reform – to lower costs, improve quality, increase access, and expand choice. But policy-makers haven’t established specific and realistic targets (represented in Step 2 in Exhibit 1) which account for the inherent trade-offs between these generic goals.
The lack of such targets has led us to our current environment where the success or failure of health policy is predictably subjective and fraught with unmet political promises. Anecdotally, public response to the implementation of the Patient Protection and Affordable Care Act (aka Obamacare) appears to have been largely influenced by two factors: personal impact (e.g., I have a pre-existing condition or my doctor is no longer in my network) and political ideology (e.g., I am against government-controlled healthcare or I think healthcare is a fundamental right). Proponents of the law cite the drop in the uninsured rate as evidence of success. The uninsured rate dropped from 14.4% in 2012 to 9.0% by the end of 2016 (Mangan, 2017) (a total 16.9 million people, including 1.1 million children gained insurance through the ACA during this period). (Clarke., Norris., & Schiller, 2017). Critics of the law point to the rise in consumer costs as evidence of the law’s failure. During the same period between 2012 and 2016, average premiums for on-exchange individual plans increased by 92%. (eHealth, Inc., 2017). Simultaneously, deductibles have increased by over 40% for these same plans and timeframes, reflecting the general trend of passing a larger portion of overall healthcare costs to patients that has been occurring over the last two decades. (Cox, et al., 2016).
And while the political discourse appears to reflect an intractable polarization and entrenched ideological division, a dispassionate analysis clearly illustrates the fact that both proponents and critics of the ACA have valid points. When taken as a whole, the statistics clearly illustrate a fundamental reality; policy changes have trade-offs and may produce both beneficial and adverse effects. In order to establish targets with broad consensus, it will be critical for politicians and policy makers to engage in a transparent dialogue about the trade-offs. While it may be difficult for politicians to admit that the US can’t offer every citizen free and immediate access to the highest quality health care in the world, it is critical they acknowledge that reality, and offer alternatives for what we can achieve through various policy options.
Performance Management Framework for the US Healthcare System
Instead of focusing exclusively on “how” to reform the health industry, we must build consensus on the objectives of reform. Without this consensus, the dialogue will remain locked in ideological assessments of “right” or “wrong” versus “effective” or “ineffective”.
For example, a proposed tactic that is intended to lower the rate of uninsured for a specific segment of the population could increase the overall cost of health insurance to society. Unless we establish how much we expect the rate of uninsured to drop and costs to rise, we have no way of assessing the effectiveness of the tactic. If we knew a tactic would cause the rate of involuntarily uninsured to drop by 50% and costs rise by 0.1%, there would almost certainly be broad public and bi-partisan support. If the reverse was true however, and a proposed tactic would drop the uninsured rate by 0.1%, but increase costs dramatically, it is safe to assume that there would be little if any support.
Clarity about targets not only establishes a common definition of success, it rallies stakeholders to action. Consider President Kennedy’s “Man on the Moon” address on May 25, 1961:
“First, I believe that this nation should commit itself to achieving the goal, before this decade is out, of landing a man on the Moon and returning him safely to the Earth. No single space project in this period will be more impressive to mankind, or more important for the long-range exploration of space; and none will be so difficult or expensive to accomplish.”
His call to action had all the key elements of SMART (Specific, Measurable, Actionable, Relevant, Time-bound) metrics. It is difficult to imagine the early space program accomplishing much if NASA had vacillated between putting a man on the moon or on Mars. The US needs a space program approach to health – we must define success.
Reconstructing the Approach to “How”
Tactics are still important of course. Once tradeoffs and interdependencies are analyzed and objectives and initial targets are established, discussions on tactics will become more focused and more productive. Consideration of adverse impacts and tradeoffs would become embedded in the policy design and implementation instead of being managed as external risk, or worse, relegated to a political messaging or public relations effort.
Strategically aligned tactics should demonstrate a clear line-of-sight to the objectives and measures the tactics are intended to impact. In the context of healthcare reform, this means that any package of interdependent policies should be assessed against the established objectives, measures, and targets. For example, an individual with a chronic condition who fails to maintain medication adherence exercises their personal choice, but also compromises the economics of the health insurance risk pool. Whether such behavior is acceptable or should be disincentived in some way would depend on an objective evaluation of the impact to the overall targets that have been established.
In situations where advocacy for specific policy position brings significant political or financial gain to an individual or party, there is a strong incentive to promote that position and minimize the importance of associated trade-offs. This dynamic makes honest dialogue nearly impossible. However, with clear, transparent, and broadly communicated tradeoffs, any argument for or against a specific policy position could be grounded in established facts gleaned from objective analysis. There would be sufficient transparency such that stakeholders would be incented to accept consequences associated with a proposed approach, rather than use them as political ammunition. An “apples to apples” comparison of a given proposal would allow for public debate over, for example, whether the tradeoff between an individual mandate and the economic cost of adverse selection is worth it - and if it is not, what approach offers a better alternative?
Debates around the potential impact of various tactics will obviously continue and will likely be driven largely by ideological differences. But there would be a built-in motivation to base positions on defensible analysis since unrealistic expectations would results in poor results and reflect on the sponsors of the position.
Conclusion
As policy positions become sufficiently quantified such that trade-off analysis is part of the implementation process, the current generation of policy makers can better advance the work of understanding the type of healthcare system we are leaving to our children. Since a framework for ongoing evaluation and adjustment of tactics does not exist, US voters currently look to a hyper-partisan political process to offer immediate solutions. In response, blunt force legislative action has become the norm – with political rancor and management of public perception as the primary tools to promote policy proposals. What is truly needed are precise and actionable measures, and a mechanism for monitoring and adjusting policy that endures beyond election cycles.
Of course, no one can predict the future with certainty, but in many ways, the performance of the US healthcare system could have been reasonably anticipated given the policies enacted and market conditions. Given the collective knowledge in areas like health actuarial models, public health trends, human behavior in market systems, and the laws of economics, variation in prediction accuracy would almost certainly decrease over time as we monitor targeted data on actual results. What is woefully lacking in the policy approach is an honest portrayal of both what is possible and what collateral impacts can be expected. In part 2, we will address the need for a mechanism to make adjustments on a more timely basis when actual results don’t match the established targets.
References
Clarke., T. C., Norris., T., & Schiller, J. S. (2017, May 15). U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. Retrieved from cdc.gov: https://www.cdc.gov/nchs/data/nhis/earlyrelease/earlyrelease201705.pdf
Cox, C., Long, M., Semanskee, A., Kamal, R., Claxton, G., & Levitt, L. (2016, October 24). Kaiser Family Foundation. Retrieved from kff.org: http://www.kff.org/health-reform/issue-brief/2017-premium-changes-and-insurer-participation-in-the-affordable-care-acts-health-insurance-marketplaces/
eHealth, Inc. (2017, January 23). Average Individual Health Insurance Premiums Increased 99% Since 2013, the Year Before Obamacare, & Family Premiums Increased 140%, According to eHealth.com Shopping Data. Retrieved from eHealth.com: http://news.ehealthinsurance.com/news/average-individual-health-insurance-premiums-increased-99-since-2013-the-year-before-obamacare-family-premiums-increased-140-according-to-ehealth-com-shopping-data
Mangan, D. (2017, February 17). The rate of uninsured Americans hits a record low as Obamacare's future remains a question mark. Retrieved from cnbc.com: http://www.cnbc.com/2017/02/14/the-rate-of-uninsured-americans-hits-a-record-low-as-obamacares-future-remains-a-question-mark.html
Paul Lichlyter Bio:
Prior to founding Lichlyter Consulting, Mr. Lichlyter was a Partner with Accenture (formerly Andersen Consulting). With over 25 years of healthcare consulting experience, Paul has been a featured speaker at several healthcare industry conferences and workshops. Paul received his Bachelor in Computer Science with a business emphasis, Summa Cum Laude, from Mississippi State University. Mr. Lichlyter holds the Professional, Health Insurance Advanced Studies (PHIAS) designation from AHIP, has served on the Advisory Board for the Children’s Home Society (CHS), and was chairman of the CHS Board Development Committee.
Jeremy Wallman Bio:
Jeremy Wallman is a management and technology consultant based in Hartford CT. Jeremy has over 15 years of experience serving healthcare, financial services, and public-sector clients. Jeremy's experience includes enterprise technology transformation, process engineering, strategic planning and strategy deployment. Jeremy is a graduate of The George Washington University and The Questrom School of Business at Boston University. Jeremy contributed to the article while a consultant at LCI and currently works as a Principal Consultant with Slalom Consulting. Jeremy also serves on the Board of Directors for the Compass Youth Collaborative.


