6 steps to transition your organization to a performance-based physician compensation model
Since the passage of the Patient Protection and Affordable Care Act in 2010, healthcare reimbursement changes are rapidly evolving from primarily volume-based, fee-for-service reimbursement to value-based, risk-sharing accountable care contracts. As a result, physician compensation models that are primarily volume-based must quickly migrate to performance-based plans that reward the "triple aim" of improved population health, better patient engagement and lower per capita costs.
The 1990s saw a period of physician employment that was primarily based on fixed salaries. In more recent employment models, the pendulum has swung from salaried to productivity-based compensation. Today, compensation models based only on productivity are being slowly replaced models that include value-based metrics. This change reflects the move toward pay-for-performance reimbursement from CMS and commercial payers. In addition, a failure to align compensation incentives with the goals of reform may increase the risk of penalties for over utilization of acute-care or diagnostic services that perhaps were encouraged by the old volume-based practice mindset.
Health systems with employed physicians primarily paid on productivity-based compensation plans face the challenge of aligning their physicians' financial incentives with the new market requirements. The article "Roadmap for Physicians Compensation in a Value-Based Market" published in the September/October issue of Physician Executive Journal provides a six-step process to help your health system navigate the complex road to a new physician compensation plan that will better align with your system strategy and market changes. The following provides a short summary of the six steps
1. Begin by creating a physician compensation committee
The first step to creating a consistent compensation methodology is establishing a physician compensation committee. Typically, this committee includes physician executives whose compensation is not affected by the medical group's compensation plan (such as the CMO who is salaried as a system executive), an executive from human resources, a senior member of the legal department and the director of physician compensation (or if this is not a current position, the director or VP of compensation and benefits). This group will evaluate the physician compensation market, review options and then approve the physician compensation plans and policies.
To assure physician input in the design, a second committee is needed — the physician compensation advisory committee — consisting of physician leaders from the medical group. This second group advises the physician compensation committee and not only provides valuable input into the design, but become the physician compensation "experts" in the medical group to help with communication and adoption of the new model.
Both committees should start with education sessions on physician compensation market data, regulatory issues related to achieving fair market value and the options in physician compensation models.
2. Move to a flexible compensation plan
Once the two compensation committees have been formed and both educated on the market data, their first item of business is to inventory the current plan models and the resulting compensation, and then compare the results to the market. The physician compensation committee will need to research compensation model options and decide how to best move the employed physician group to a more consistent plan that is fair, equitable (especially inside a specialty), aligned with system goals and easy to administer.
In view of current changes in provider payment reimbursement, the new compensation plan will need to be capable of evolving over time. The physician compensation plan should parallel payer reimbursement changes by having the physicians being paid increasingly on clinical outcomes and efficiencies in care as productivity is "de-emphasized." Flexibility to increase the percentage of incentive and other non-productivity dollars as payer reimbursement moves to more value-based payments is essential to achieving physician-system alignment and must be part of the new plan. For systems that are not yet involved in value-based contracting, adding a pay-for-performance incentive plan is still a good way to start the transformation.
3. Build your primary care compensation plan first
As primary care physicians move to a team-based, coordinated care model with patient-centered medical homes and medical neighborhoods, the need to eliminate productivity-based compensation models is most acute. The compensation model for primary care physicians should promote "teaming" and outcomes, not independence and volume. To achieve good outcomes, primary care physicians will need to work proactively with the patient and specialists to coordinate care. These required changes in the care model are compatible with the findings of the report of the National Commission on Physician Payment Reform that concluded that two of the reasons for the high level of expenditures in our healthcare system are (1) reliance on technology and expensive care and (2) a high proportion of specialty care. Coordination and new models of care by primary care physicians will improve the value for patients. The compensation plan for the primary care physician needs to strongly support these changes.
To promote this focus on coordinated team care and chronic disease management, compensation plans for primary care physicians should include (1) a guaranteed salary based on years of experience, (2) incentives for access, clinical quality, service quality, efficiency, productivity and citizenship as well as (3) a panel management fee.
4. Take advantage of existing metrics
There are numerous Healthcare Effectiveness Data and Information Set and Physician Quality Reporting System metrics that are currently defined and benchmarked, which can be applied as early incentive metrics for the clinical and service quality components of the incentive portion of the plan. The panel management fee compensates the primary care physician for the additional time spent working with the care team to provide evidenced-based, coordinated care for the more severely ill patients as well as assuring that all appropriate preventive care measures (e.g., immunizations, well visits, cancer screening) are completed for all patients in the physician's panel. As the medical group and health system move to increased value-based and fixed payment reimbursement, this new reimbursement model will most likely be based on the population size and severity of disease. It still makes sense to have a portion of the physician's incentive based on productivity or panel size to encourage the primary care physician's alignment with the health system's financial and market share goals. However, the primary focus of primary care physician compensation must reward excellent patient access to high-quality care at the lowest reasonable cost.
As systems become more adept at measuring patient-centered outcomes, the incentives will need to move from the more typical process metrics now dominating HEDIS and other commonly used quality metrics to those measuring outcomes that matter to patients.
Although metrics and data for incentives are typically more robust for primary care physicians, specialty incentives should be quick to follow. With a recent movement in patient-centered specialty homes, there is an opportunity to develop compensation incentives related to referral management and coordination of care or even PCSP certification. Specialty divisions should work with the physician compensation committee to develop specialty specific quality, cost and service metrics.
5. Maintain continuous communication and an open feedback loop
It is important to communicate and involve your employed physicians in the changes required of their practices from healthcare reform and the changes in payer reimbursement. You need their input and their willingness to change clinical care models to help you cross the "crevasse" from volume to value.
Communication can take the form of large "town hall" educational lectures by experts in the field or small practice meetings that allow more questions. Hospital administrators should be transparent with their employed physicians about the multiple pressures that are decreasing revenue streams and the new world of measurement that is driving the need to focus on improvements in quality outcomes and efficiencies of care, which in turn requires a change in the compensation model.
6. Consistently move to more performance-based compensation
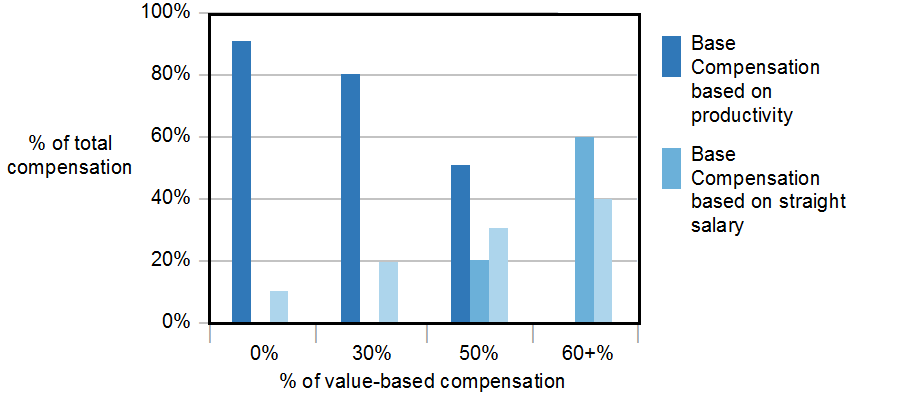
The move to a model of salary plus performance-based compensation does not happen overnight. As the medical group or health system begins to increase the percentage of value-based contracting, the game changes and there will be more emphasis on the cost savings and quality metrics that should be strategically linked to the payer contracts as well as the health system quality and safety goals. As the value-based reimbursement grows to 25 to 30 percent, the percentage of the physician's compensation plan based on performance-based incentives also needs to increase proportionately.
When the group moves to a position where the majority of revenue (> 50 percent) is from value-based contracts or full capitation, the physician compensation is best managed with a base salary model based on the physician's experience and specialty and a performance-based incentive plan that is 30 to 40 percent of the overall compensation. This incentive can include a portion based on productivity (to ensure the volume of patients in the medical group is adequate and growing) and the remainder should be based on numerous quality outcomes and efficiency metrics that are aligned with the system's strategy. By this time, the group will have the processes in place to report the quality, efficiency and productivity data to the physicians in a timely and accurate manner. With the improved communication plan, the employed physicians should be well versed in the strategy and goals of the health system at this point and comfortable with the culture of measurement and transparency.
Below is a graphic representation of the changes in the compensation plan as the value-based reimbursement increases (see Figure 1).
Figure 1
Summary
The goal of the physician compensation plan is to encourage and support a transformation of the care model that leads to improved health of the patient population and outstanding organizational performance in a value-based environment. The challenges of paying for outcomes instead of volume are many, but a deliberate, steady and evolving approach will allow an employed medical group to transition to a compensation plan that is aligned with value-based reimbursement from payers and supports the strategic goals of the organization. This change in physician compensation culture must start now.


