A holistic approach to problem solving is necessary to address the complex issues facing healthcare providers today. Despite the demands of the current environment, quality must remain the top priority. A robust quality measurement and improvement program can help you achieve your quality objectives and clinical documentation improvement is a critical piece to a holistic approach to quality.
When a gunshot victim arrived at the emergency department of an academic medical center in hemorrhagic shock, clinicians sprang into action to provide immediate, potentially life-saving treatment, administering several liters of fluid, more than 26 units of blood and other support measures that ultimately helped save the patient’s life. Later, when the clinical documentation team looked at the patient’s medical record, “hypotension” was how the clinical picture was described to support the fluid resuscitation and blood administration. “Hemorrhagic shock” did not appear in the clinical documentation. The potential ramifications of incomplete or inaccurate clinical documentation are significant. It can negatively reflect the quality of care, potentially leading to longer lengths of stay, lower expected mortality scores, higher readmission rates and increased care costs. It also can contribute to claims denials.
However, studies show that clinical documentation could be improved, on average, in more than 50 percent of medical charts. A number of factors contribute to incomplete or inaccurate clinical documentation, including provider time constraints and a knowledge gap between medical language and coding nomenclature, coupled with sporadic training on how clinical documentation impacts coding and claims reimbursement.
“To the providers, it was obvious that the patient had hemorrhagic shock and provided the appropriate care,” says Hunt. However, when documenting the diagnosis, that term was not entered. “When you’re trying to save a life, worrying about using the right words isn’t top of mind.” Coding specialists, who are trained in medical terminology, cannot translate the information in the medical record. “Either the provider uses the words needed for accurate and complete coding or the codes do not reflect the true picture of complex medical decision making,” says Vizient Principal Angela Hunt, RN, MBA, CCDS.
Accurate and complete clinical documentation matters
It is vital to choose the words that accurately describe the acuity and complexity of the patient. “An accurate and detailed record is essential for translating the patient’s story into coded data necessary for care delivery, publicly reported quality outcomes, proper reimbursement, physician report cards, public health data and more,” says Hunt.
Clinical indicators need to be clear in medical records to support documented diagnoses. As value-based care continues to gain traction, it requires that providers collaborate closely on a patient’s medical management. Accurate, complete and specific clinical documentation will be more important than ever to keep the care team updated on a patient’s condition and allow them to identify and address gaps in care. “The quality of documentation speaks to the risk of mortality, length of stay and cost of care,” says Hunt. “Providers need the right tools to streamline complete and accurate documentation of diagnoses.”
Fortunately, solutions are available to help physicians and advanced practice providers improve clinical documentation.
Technology solutions boost clinical documentation improvement
Supporting providers with clinical documentation tools can help reduce incomplete or inaccurate documentation. The right tools can also reduce the need for coding specialists to query physicians to clarify diagnoses or capture missing information.
“It’s important to get to the right diagnosis more quickly with less interaction between providers and clinical documentation improvement nurses and coding specialists,” says Hunt. “That frees up doctors to do what they do best, provide patient care.”
Several emerging technologies are attempting to address the challenges of clinical documentation. Artificial intelligence innovations marry data points, such as lab results, vital signs and clinical words in the patient record and provide clinical documentation suggestions to the provider. Computer-assisted analyses of physician documentation provide real-time feedback and attempt to resolve inaccuracies. Prioritization software identifies and prioritizes potentially problematic charts to help CDI staff focus their efforts. Data analytics can provide actionable comparative benchmarking insights to drive clinical documentation improvements.
Another tool, pocket-sized documentation tip cards, help physicians remember key documentation points, from documentation basics to severity clinical indicators. While tip cards are a valuable tool to help providers document diagnoses correctly,they’re often left at home, misplaced or damaged.
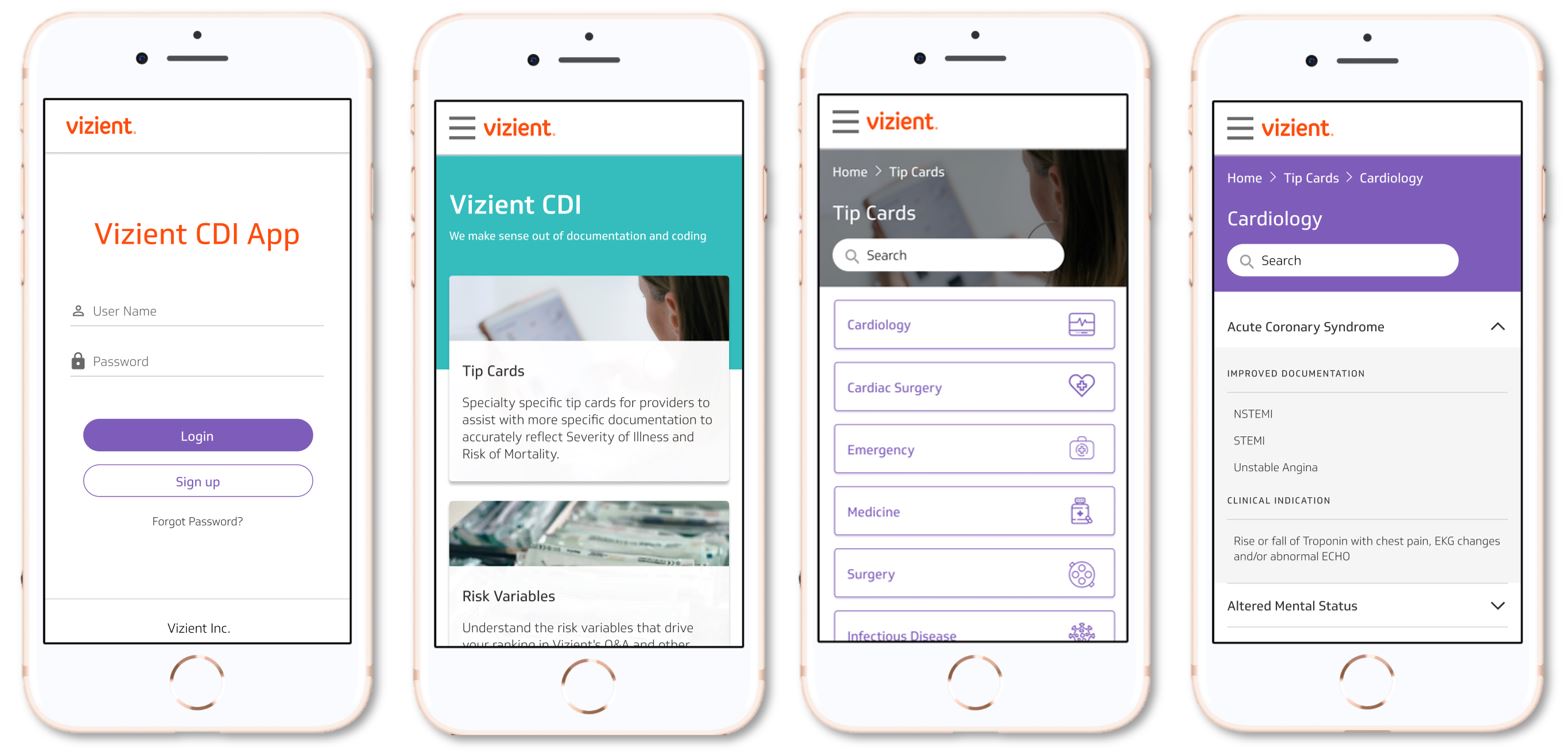
Vizient is launching its clinical documentation improvement CDI app, which helps physicians and advanced practice providers document the most common diagnoses in inpatient hospital settings by providing access to tip cards via smartphones. The electronic tip cards are broken out by nine service line categories and allow providers to search for a particular diagnosis or an abbreviation. The app enables the physician to quickly move past the incomplete nomenclature to the correct and accurate documentation for the diagnosis. For example, in the case of the gunshot victim, typing “hypotension” into the app would have displayed a list of all the hypotension documentation possibilities with the specificity needed for coding specialists to use the right codes, including the critical hemorrhagic shock information.
“Vizient’s CDI app adds to the providers’ toolbox concurrently while other technologies intersect with clinical documentation staff and coding staff,” says Hunt.
Hunt adds that an update to the CDI app, planned for release in late 2022 will include Vizient’s risk model variable definitions and Hierarchical Condition Categories to help accurately document the complexity of care for patients with serious acute or chronic conditions.
As clinical documentation requirements grow more complex, technology solutions can help health care organizations achieve their CDI goals. Hunt says any tool should be user-friendly for busy providers. “We don’t see clinical documentation getting easier,” adds Hunt. “The tool you adopt should shorten the time it takes for providers to complete clinical documentation and minimize queries from the CDI or coding team.”
At Vizient, we are committed to helping our members transform care delivery by bringing our experts to your experts and turning data into action. Our comprehensive Operations & Quality discipline includes specialty areas such as labor and operational efficiency, clinical quality, safety, care variation and clinician engagement. Our strategy is focused on integrating our capabilities into services that advance provider results using our industry-leading data and analytics combined with our subject matter expertise.
At Vizient, we are committed to helping our members transform care delivery by bringing our experts to your experts and turning data into action. Our holistic approach to a clinical operations and quality improvement program includes specialty areas such as labor and operational efficiency, clinical quality, and high reliability. Our strategy is focused on integrating our capabilities into services that advance provider results using our industry-leading data and analytics combined with our subject matter expertise.
Additional information about the Vizient CDI app and other solutions to improve your clinical documentation accuracy and quality is available online.


