With final rule on the Medicare Access and CHIP Reauthorization Act now in hand, physician practices across the nation are preparing for the most dramatic healthcare payment reform this generation has seen.
MACRA and its associated Quality Payment Programs replace former Sustainable Growth Rate provisions for physician Medicare reimbursement and signal the industry's tipping point in the move to value-based care. Fee for Service Models in place today will quickly transform to reflect the seriousness of a cost-conscious era of quality-based reimbursement.
Research conducted in early 2016 suggests that only 43 percent of practices have compensation tied to quality or value of care heading into MACRA. The study also cites regulatory and paperwork burden as the biggest deterrent to practice satisfaction among physicians. The Centers for Medicare and Medicaid Services new policy framework, more than eight years in the making, works to address those concerns, combining several previously unintegrated healthcare reporting initiatives into a unified QPP that most healthcare providers will qualify for.
With pick-your-pace options, flexible measure selection, reporting period flexibility and small-practice provisions cemented by the final rule, providers have a unique opportunity to engage new value-based strategies slowly without penalty. The march toward MACRA is officially underway. This article lays out four key focus areas to help providers successfully navigate the new pay-for-performance model in 2017's inaugural reporting year: financial, clinical, technical and staff training.
Understanding the MACRA landscape: two paths to participation
Under MACRA, eligible clinicians can begin collecting performance data on care given and technology utilized anytime between Jan. 1, 2017 and Oct. 2, 2017. Data captured by providers during the 2017 reporting period is due by Mar. 31, 2018. Eligible clinicians have two reporting track options to participate in QPPs under MACRA which are the Merit-based Incentive Payment System and the Advanced Alternative Payment Model. Of those eligible clinicians, 90 percent are expected to participate in MIPS and 10 percent in APMs
MIPS: This QPP option combines outcome and quality-based payments with reduced fee-for-service reimbursement. MIPS integrates three payment programs—the Physician Quality Reporting System, Meaningful Use, and Value-based Payment Modifier—with an assessment of clinical practice improvement initiatives to establish an annual Composite Performance Score that reflects a physician's standing relative to reporting peers, on a scale of 1-100. That score determines Medicare incentive or penalty payments for physicians at a 4 percent adjustment rate starting in 2019, and up to a 9 percent adjustment rate by 2022.
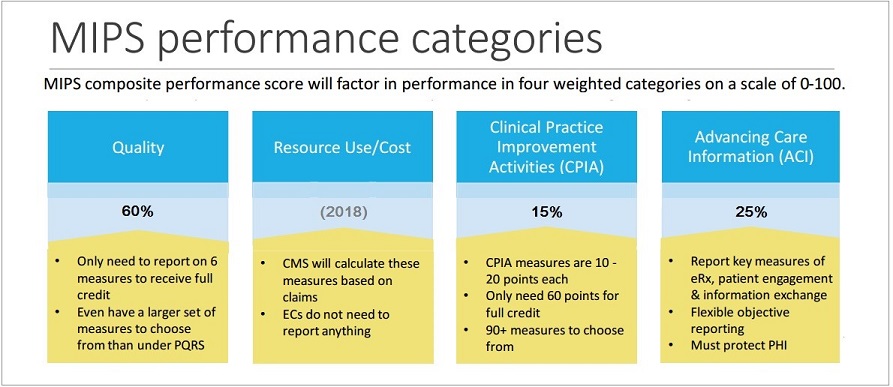
While cost will be tracked by CMS in 2017, cost category determinants will not be factored into payment adjustments until 2018. Under MIPS, providers can choose quality reporting objectives and measures that best align with medical practice specialty and workflow specifics. Only physicians practicing under Medicare for the first time in 2017 and those who anticipate billing less than $30,000 for fewer than 100 Medicare Part B patients are exempt (unless of course you are in a CMS Advanced APM).
Clinicians have four "pick-your-pace" avenues for payment program participation in MIPS:
Option 1: Nonparticipation
Providers who do not submit 2017 QPP data will suffer a 4 percent negative payment adjustment.
Option 2: Submit partial data
Providers who submit QPP data on at least one quality measure or improvement activity, or the required measures in advancing care information can avoid a negative payment adjustment.
Option 3: Partial reporting period
Providers who submit more than one quality measure, more than one improvement activity, or more than the required measures in advancing care information for a period of 90 days can earn a neutral or small positive payment adjustment.
Option 4: Full reporting
Providers who submit for a full 90-day period or a full year of 2017 data in all categories may earn a moderate (or full) positive payment adjustment.
Clinicians can report MIPS data independently or with a group entity. For the initial transition year under MIPS, reporting thresholds have been lowered and an additional $500 million has been provisioned annually for "exceptional performance" bonuses to clinicians who achieve a final score of 70 or higher.
Advanced APMs: The second category of QPP under MACRA is Advanced APMs. Less than 10 percent of MACRA-eligible providers are expected to qualify for an Advanced APM in the first reporting year under this regulation. Physicians who qualify to report under an Advanced APM get a 5 percent bonus each of the first six years of MACRA, and base payment updates higher than those under MIPS from 2026 onward, when the reporting party earns significant revenue (25 percent) or sees sufficient patient volumes (20 percent) through qualifying Medicare or payer models.
Payment adjustments based on 2017 performance data will go into effect on Jan. 1, 2019. The MACRA final rule provisions $20 million each year for five years to fund training and education for small practices of 15 or fewer clinicians and practices in rural areas.
Four keys to navigate the transition
Implementing a comprehensive strategy is critical to provider success under MACRA. Assessing infrastructure before layering in payment program initiatives ensures future plans are built on a solid foundation. Practices should focus on four areas in evaluations and strategic planning: financial, clinical, technical and staff training.
Financial success
The best place to start when evaluating infrastructure is the existing revenue cycle. Stabilize and optimize revenue streams to ensure the practice isn't leaving money on the table. Renewed emphasis on accurate coding, documentation support, self-audits and denial management can help plug revenue leaks, potentially shoring up funds that may serve the practice elsewhere. It's important to understand key performance indicators, trending and the cost of operation heading into QPP participation.
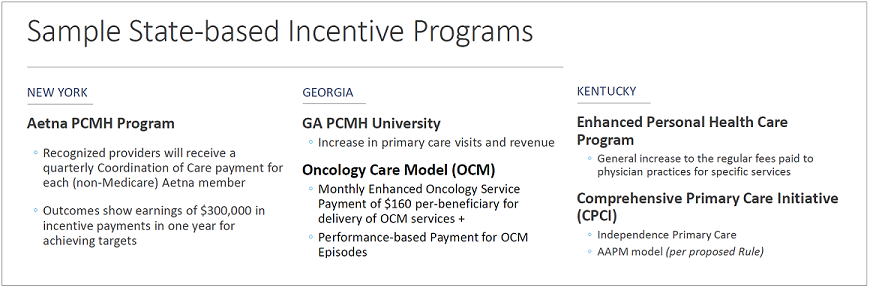
Providers should know how to scrutinize their payer reimbursements. Analyze contracts and variance rates to ensure revenue due to the practice is collected. It's also important to understand any value- and risk-based contracts a practice may qualify for. Reach out to the commercial payers engaged with the practice to determine what is available in the area. Many plan-specific and state-based incentive programs that exist are not advertised.
Clinical success
With performance on quality targets accounting for 60 percent of MIPS scores in the first year of QPP, quality measures will be an essential aspect of success. Understanding where the practice has performed strongly in previous years and aligning those services to MIPS measures, will influence quality measure focus going forward and can help practices be competitive. Take advantage of measures that appear across multiple categories to reduce reporting burdens.
Population health and care coordination are at the heart of QPP models. Focus on expanding communication with beneficiaries and patient care teams as well as specialists. Much of the care coordination measures center around collecting and sharing patient information with care teams, referred providers and the patient themselves. Optimize outcomes by partnering with facilities across the continuum of care. Be consistent in using existing functionality for electronic data exchange and messaging or identify new, cost-effective opportunities for patient engagement, communication, education and empowerment.
Technical success
Technology infrastructure is paramount to reporting under MACRA. Establish a firm understanding of the measures and the existing EHR functionality that is available to track for the adopted payment model. Practices will need to integrate data from financial and clinical sources to monitor and report on required measures and factors. In many instances, we have found that providers have not been able to optimize the most recent functionality enhancements in the EHR and health IT systems they already have.
In some cases, EHR template and workflow customization as well as dashboard creation can help practices quickly and routinely target measures and KPIs pertinent to practice objectives. Test the process for submitting reporting metrics ahead of time, streamline workflows and leverage technology wherever possible to create efficiencies for patient engagement and throughput.
Staff success
Securing inside expertise on new payment models, health information management and technology implementation is a major challenge for practices today. Practices need to align with partners who can help shoulder the burden of expertise and implementation, educating practice stakeholders along the way while still allowing them to focus on patients as priority number one. Look for partners who will keep practice staff informed, proactively evaluate payment models, offer coaching on how to go engage payers and help management flesh out strategic initiatives.
Involve and educate appropriate staff members at different points in the planning process and make sure the team has a collective general understanding of practice objectives so everyone is working toward the same goals. Take advantage of resources such as Medicare's Physician Compare and Quality Resource Use Reports to benchmark and compare physician performance and reporting practices.
Moving past provider hesitation
Competing priorities, limited resources and general unfamiliarity with MACRA and the final rule have contributed to market hesitation to embrace reform, even with MACRA's commencement close at hand. That said, there will not likely be a more ideal time for physicians to prepare for the QPP transition.
Flexible, scaled participation options mean physicians can stave off first-year losses and potentially earn incentive and bonus payments via partial reporting as clinicians learn to navigate the new system. In rewriting policy, close attention was paid to identifying quality measures that were applicable across multiple models to incentivize providers for improving outcomes while simplifying the reporting process. Diminished reporting data thresholds have been implemented during the first reporting year. CMS also built in small and rural practice training resources to counter market concern.
Care providers who proactively engage with new payment and care delivery models, and cultivate the right partnerships and expertise, will unequivocally have more opportunity in the future. These three steps quickly engage stakeholders and establish proactive momentum for the MACRA journey:
• Take advantage of every resource available to learn about QPP specifics and support practice efforts
• Engage partners with the needed expertise or designate internal resources to lead the charge
• Establish a strong game plan that begins by January 2017
The average practice can easily qualify for incentives under the new QPP, but many lack the internal resources necessary to succeed under MACRA. Proactive leadership and expert partnerships are essential to juggle the new initiatives and cultivate a value-based business strategy. Look for partners that will go "at-risk" with you. Tie them to your success, that way everyone is guaranteed to win.
Embracing a business approach for value-based care
There is real opportunity for practices to be a catalyst for change within communities. Patient growth, panel participation, partnership opportunities and care model invitations are among the benefits that proactive practices stand to reap, all of which could have big implications for coordinated care and population health initiatives. Practices that lead the charge, participate in broader patient and community engagement and grow the care ecosystem will have the long-term advantage.
About the Author:
Justin Barnes is a nationally recognized business and policy advisor who serves as Chairman Emeritus of the HIMSS EHR Association as well as Co-Chairman of the Accountable Care Community of Practice. As Chief Growth Officer with iHealth, Justin assists providers with optimizing revenue sources and transitioning to value-based payment and care delivery models. Justin has formally addressed Congress and the last two Presidential Administrations on more than twenty occasions on the topics of MACRA, value-based medicine, accountable care, interoperability, consumerism and more. He is also host of the weekly syndicated radio show "This Just In."
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker's Hospital Review/Becker's Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.


