Health care organization leaders are working hard to create, update and continuously improve on their processes to align with the Triple Aim initiative (see Figure 1. Triple Aim Model).
Their top priorities include providing appropriate levels of patient care and patient care quality, as well as learning about patient and health plan member populations and optimizing costs for health care delivery. Since these priorities are so focused on process efficiencies and patient health management outcomes, health care leaders are learning from and implementing Lean methodologies, which focus on understanding and improving customer value. In the case of health care, this means a focus on value to both patients and providers.
This article offers considerations for health care leaders to adapt Agile Management (Agile) as their framework for supporting clinical and/or operational process improvement projects. Agile offers an effective framework to organize and control process improvement projects, especially when paired with a prototype re-engineering approach.
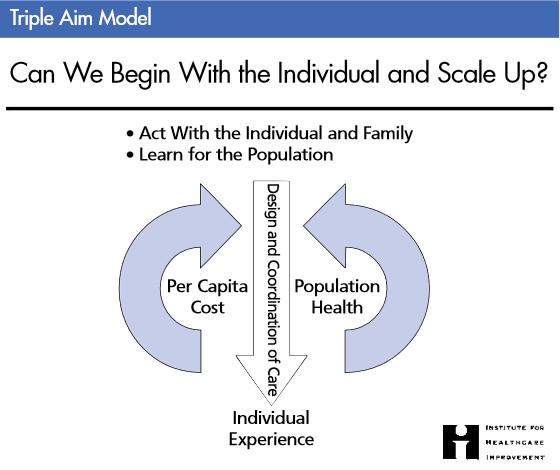
Figure 1. Triple Aim Model
Health care organizations are investing in continuous process improvements to align with the Triple Aim model, so a relevant project management methodology like Agile can potentially maximize new process benefits and return on investment.
What Is Agile?
Perhaps you have already heard of Agile and its related terms like "scrum," "iterative development," "sprints," and "user stories." The term "Agile" rose out of a team-based iterative software development methodology. Agile's software industry-based heritage differentiates it from Lean, which originated in the manufacturing industry.
The framework has proven successful in software development, especially for situations in which a Product Manager and the Agile team use this iterative methodology to discover the solution. Likewise, Agile can be adapted to operational or clinical process improvement projects in health care.
Agile is basically a model containing process groups run sequentially within a defined period of time or "iteration," and with a feedback loop to the customer for solution validation. The solution can be "discovered" or defined in detail through iterations that deliver functions and features of the solution. Thus, agile project management is an approach that leverages this iterative model to define and control the project work.
When Is Agile a Good Approach?
Agile can potentially be beneficial to healthcare projects under the following scenarios:
1. When most, but not all, of the solution, is understood. Start with the goal of the process. The goal needs to be specific and measurable. For example: "The new utilization management review process will reduce Medicare claims denials by 50% within 60 days of its implementation."
a. We recommend using an impact map to visualize the goal and stakeholders, how stakeholders' work will be affected by process changes, and what is changing (at least at a high level).
2. When you believe or suspect there may be a number of scope changes for unknown areas of the solution.
3. When you want process stakeholders to participate in developing the solution.
4. When you want assessment and evaluation of the impact of alternatives.
5. When there is not a hard deadline for the solution; that is, there is time to "discover" the solution through iterative work.
Agile Strengths and Weaknesses
The strengths of Agile include:
1. No wasted time on non-value-added work. Process functions, roles, and steps are validated in sponsor review sessions.
2. Avoiding all management issues due to formal scope change requests. The process components that the team develops are validated by the sponsor in the end-of-iteration reviews.
3. No wasted time planning uncertainty. Since the sponsor defines an iteration's work, the work is planned within a two- to four-week iteration and subsequent iterations. The team develops the work plan.
4. Providing maximum value within time and cost constraints. Many studies have shown that Agile has the potential to deliver value in conditions of solution uncertainty much faster than traditional project management.
There are also some important weaknesses or constraints with Agile to keep in mind:
1. Requires meaningful stakeholder participation (or "customer" participation);
2. Agile cannot define what will be delivered at the end of a project.
3. Agile requires a strong team of process subject matter experts.
4. No "Scrum Master" role. Unlike with software development teams, in healthcare there is likely no one who is coaching the team on Agile practices, such as defining work in iterations. This is where a subject matter lead role, sponsor, or even project manager will need to lead.
5. The team needs to function at a high level, and thus requires experienced team members with high levels of demonstrated professionalism.
Agile Project Management Process Outline
Following is a best practice model for prototyping a process improvement project using Agile (see Figure 2. . Prototyping a new or significantly altered process is an effective way to discover optimal functions, procedures, and role responsibilities in order to maximize process goal attainment.
Prototype process engineering paired with Agile helps to quickly confirm incremental requirements, benefits, and deliverables. Incremental delivery can be an excellent strategy for calibrating and managing the change impact on your organization while effectively managing your project budget. The following diagram presents a high-level method for organizing this work:

Figure 2. Agile Prototyping Process Model
In summary, health care organizations may want to consider using Agile to organize and control their process re-engineering initiatives. This Agile framework is presented as an adaptive methodology that situates the Product Manager, Sponsor and the team to co-discover and elaborate processes and their requirements in situations where this work has significant ambiguity. Agile enables the project team to deliver value to the business early in the project's lifecycle thus increasing the ROI of the project investment.
Chet Stagnaro joined Freed Associates in 2011. Chet has significant experience in PMO, Program and Project Management.
Prior to his position with Freed, Chet was a Program Manager with the University of California, San Francisco, a prominent medical and healthcare research institution. He also has experience in IT PMO and portfolio management in healthcare IT. In his career, Chet has worked with healthcare, higher education, financial, energy, manufacturing and international distribution service sectors in project management and general management roles.
Chet holds a Doctorate in Management, Organizational Development, from Colorado Technical University. He also holds a Master in Information Systems from the University of Phoenix and a Master in Business Administration from the Monterey Institute of International Studies.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker's Hospital Review/Becker's Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.


