Hat tip to Sharon O'Keefe, CEO of the University of Chicago Medical Center, for introducing the phrase "make your assets sweat" to our team, which inspired me to write this article.
The Affordable Care Act, increased government regulations and rising healthcare costs are forcing hospitals to do more with less. Last year, several major healthcare networks took drastic steps to mitigate the financial stress: layoffs, consolidation and downsizing operations. While such large-scale changes may seem like the obvious way to react based on visible P&L line items, I believe that hospitals can do better by solving one of the root causes of low operational productivity: the underutilization of expensive assets.
The Elephant in the (Operating) Room
Idle time is perhaps the most underrated metric in hospitals. Study after study finds that the most expensive resources are often underutilized. It is widely estimated that the true utilization of ORs at many hospitals is less than 65 percent — however, the method of calculating utilization often masks the real number. The value of OR time can be up to $6,000 per hour. Unlike a well-run manufacturing plant, most hospitals don't establish a rigorous methodology to understand the true utilization of their assets and the sources of "leakage." They tend to be satisfied with the current definition of the utilization metric rather than digging deep to find and plug each source of leakage.
Broadly, there are four buckets of "resource utilization leakage":
1. Schedulability. If we choose to run an expensive resource such as an operating room from 8 a.m. to 5 p.m. on weekdays, we have implicitly decided that this particular asset only needs to work for 45 hours each week. On paper, our utilization might look great since it is reported as a percentage of those 45 hours. Obviously, it is not feasible to use all 168 hours of the week (since it is unlikely that we could realistically conduct surgeries at 2 a.m. on a regular basis). However, it might be possible to keep the ORs open for 4-5 additional hours each day, which would create a lot more capacity. The key question is "Are we making our assets sweat?" At $6,000 per hour in potential revenue, that could be tens of millions of dollars of foregone revenue based on an asset utilization decision that may have been made years ago based on a different demand profile.
2. Availability. Even when a resource appears to be available, it is often not really available because it needs to be cleaned, changed over or serviced. This causes "availability leaks" which further reduces the time available for the resource.
3. Productivity. This is often the hardest to catch. Sometimes, an insufficient demand, such as a light caseload for the OR, can be the underlying reason for a low productivity metric, in which case there is nothing that the operational team can do to improve the metric. At other times, it might be that some of the necessary tasks, such as turning the OR over between cases, run for longer than planned. It is also possible that getting the first case started is chronically late by 15-20 minutes each day, creating a domino effect on the cases scheduled for later in the day. These small productivity leaks are like grains of sand — easy to slip through your fingers, but collectively, they can add up to a significant impact. If things run just a little bit quicker on every action, the gross output of the resource can be a lot bigger than we might expect. For example, by turning a plane around at the gate in 30 minutes (rather than the 45-50 minutes observed at most other airlines), Southwest is able to get one extra flying leg per day for many of its 737 aircraft. The choreography required to turn a plane in 30 minutes including fuel, bags, passengers, crew, beverages, etc. is hard to do — yet they do it consistently thousands of time each day across the country. The impact of this "small amount of productivity" on the incremental revenues and asset utilization is one of the reasons that Southwest is one of the only airlines to have been consistently profitable over a 43-year period.
4. Quality. Last but not least, if something needs to be repeated because it wasn't done right the first time, it leads to "quality leaks" and capacity waste. Capacity is as perishable as a seat on a plane. Once the 7 a.m. flight on February 16 leaves with an empty seat, there will never be an opportunity to recapture it. In an OR context, a quality leak in the OR may manifest itself as the need for more follow-on visits than strictly necessary. Thankfully, this is usually not the biggest source of utilization leakage in most hospitals.
To Really "Make the Assets Sweat," We Need Lean Methodologies and Predictive Analytics
Traditional dashboards and business intelligence tools enable dynamic drilldowns into every aspect of operational performance. There are excellent visibility tools that clearly and consistently communicate actual performance to the leadership team and across the organization. However, they fail to provide the forward-looking view and intelligent set of recommendations to achieve a better operational outcome. Dashboards are like glorified scoreboards — you can't expect your team to win the Super Bowl simply because the owners installed a fancy new digital scoreboard with real-time data feeds that provide updated statistics within seconds of each completed play.
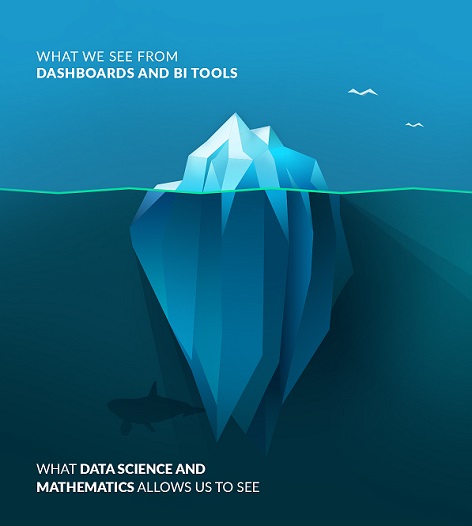
The good news is that the recent investments in EHR and data warehouses over the last few years have created the necessary foundation of data from which forward-looking views based on deep data science and predictive analytics can be built. Such approaches can mine historical utilization patterns and develop appointment models that match supply and demand patterns in a fine-grained manner to improve schedulability, availability, productivity and quality. Optimizations like these are never a "once and done" approach; patient treatments are inherently highly variable and patient-specific. Hence, the optimization approach must make it easy to facilitate last minute swaps and exchanges to keep the operations flowing smoothly while also using machine learning to monitor the actual-versus-expected resource utilizations — and to periodically tweak the templates to continuously improve operational performance.
The optimization approach most likely to drive impact depends on multiple factors, including:
• What proportion of the demand is "walk in" versus scheduled in advance?
• What is the variability of the treatment time across patients (i.e., is it a tight band where most treatments are +/- 15 percent of an expected length, or does it vary widely as in infusion treatments that can have a 30-minute treatment and a nine-hour treatment)?
• How "fungible" are the assets being scheduled? An infusion chair may be like any other infusion chair, but a provider is a very specific asset, as is an imaging machine that can do a very specific set of imaging procedures.
The demand pattern analysis must be done to within the most granular time interval that makes sense (e.g., 15 minutes, 30 minutes or an hour). Longer time intervals (e.g., number of treatments per day or per week) are gross averages and simply do not address the core operational issue. For example, assume that the freeways are completely idle all evening except for a two-hour rush hour period during which 100,000 cars are on the road. It is not useful to conduct "averaging analysis" over the entire evening (4 p.m. to 9 p.m.) and conclude that the demand was only 20,000 cars per hour and that the freeway capacity ought to easily handle such a load.
The supply-side analysis should ensure an adequate supply of assets (people, machines, rooms, chairs, etc.) to match the incoming demand pattern of patient appointments. This is usually a constraint-based optimization problem where the available supply has "rules" based on the hours of operation, skill requirements, coverage levels required to perform the treatments safely and effectively, etc.
The purpose of the demand- and supply-side analysis is to determine the approach that creates the most operational stability — hour after hour throughout the day. This might require building queueing models to determine the schedule of nurses and technicians, or it may require the creation of optimal templates that steer the right patient into an appointment slot of the right duration at the right time of the day to create the flattest utilization profile from all of the patients who are being treated at the same time in the specific unit. For OR blocks, it requires predicting the caseload (volume and mix) for each surgeon over the next 90 days and accurately determining the right number to meet the expected case load, while satisfying the constraints of staff, equipment and room availability.
Assigning the right resource to the right user (patient and/or provider) at the right time on the right day is a complex mathematical problem. The conventional first-come, first-served model of scheduling appointments in the EHR simply doesn't work. It is a "portfolio optimization problem." Just as a financial advisor cannot be expected to make a recommendation for you to buy a stock without a detailed understanding of the other stocks in your portfolio, a scheduler cannot be expected to make a recommendation for the optimal time slot to be given to a patient without an understanding of the "portfolio" of patients who will be undergoing treatment at around the same time in that treatment unit. This is because the duration of each type of treatment will vary, and optimization requires phasing the starts and stops of the various treatment types to achieve as flat a utilization profile as possible for most of the day.
At LeanTaaS, we have had an opportunity to build and deploy software products that co-exist with the EHR and have delivered substantial improvements using these concepts across a variety of settings:
• Operating Rooms: By looking at OR case data and block data, predictive analytics can help understand utilization patterns, such as which surgeons have more time than they need and which surgeons need more time than they have, and suggest block schedule changes based on objective facts — after taking surgeon and staff preferences into consideration. In addition, mobile block exchange (MBE) enables surgeons and their schedulers to release and request blocks that help improve utilization even further. In fact, UCHealth has seen a 16 percent increase in OR utilization since implementing LeanTaaS' iQueue for Operating Rooms solution. This "continuous smart block allocation" makes "operating rooms sweat" by ensuring that during every possible hour the OR is being put to the highest and best use for which it is capable.
• Infusion Centers: By looking at historical demand patterns and operational constraints, sophisticated forecasting algorithms can predict the daily volume and mix of patients and orchestrate appointment slots such that the chair utilization ramps up smoothly, stays flat for most of the day and then ramps down smoothly. This can increase the number of patients seen by 10-15 percent while simultaneously reducing the wait time at the midday peak by 30-50 percent.
• Labs: By analyzing the arrival pattern for lab draws, the queueing models were able to determine the optimal staffing of phlebotomists and nurse technicians to reduce the wait time for patients from an hour to less than 10 minutes at a leading cancer center.
Predictive analytics and optimization algorithms are not a "nice to have" or exclusive province of academic institutions. They are essential. Customer satisfaction experts often say "a smile on the face of the taxi driver cannot compensate for the negative experience created by his cab breaking down." Similarly, hospital executives need to come to grips with the fact that "an overzealous process improvement or coordination effort cannot compensate for the fact that the appointments were not created in an optimal manner." It is a bit like dealing a bad hand to a world-class poker player every single time; there is only so much they can do with it. By contrast, dealing a perfect hand to a novice poker player will consistently have winning results.
It takes predictive analytics, optimization algorithms and machine learning to set up the calendar of appointments for all resources in an optimal manner. The data finally exists and is accessible. The algorithms are known and are increasingly being embedded into products. We can all look forward to an ever-increasing improvement in the smoothness of the operational flow in hospitals over the coming years.
###
Mohan Giridharadas is an accomplished expert in lean methodologies. During his 18-year career at McKinsey & Company (where he was a senior partner/director for six years), he co-created the lean service operations practice and ran the North American lean manufacturing and service operations practices and the Asia-Pacific operations practice. He has helped numerous Fortune 500 companies drive operational efficiency with lean practices. As the founder and CEO of LeanTaaS (a lean and predictive analytics company), Mohan has worked closely with dozens of leading healthcare institutions including Stanford Health Care, UCHealth, UCSF, Wake Forest and more. Mohan holds a B.Tech from IIT Bombay, MS in Computer Science from Georgia Institute of Technology and an MBA from Stanford GSB. He is on the faculty of Continuing Education at Stanford University and UC Berkeley Haas School of Business and has been named by Becker's Hospital Review as one of the top entrepreneurs innovating in healthcare. For more information on LeanTaaS iQueue, please visit https://iqueue.com/ and follow the company on Twitter @LeanTaaS, Facebook at https://www.facebook.com/LeanTaaS and LinkedIn at https://www.linkedin.com/company/leantaas.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker's Hospital Review/Becker's Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.

