For the last decade, CIOs have been consumed with implementing and gaining adoption for EHRs. Now that they are implemented and widely adopted, we've arrived in the "post-EHR era" — and the CIO's role is shifting.
Now, the CIO's main responsibility is to make all of the data collected day in and day out throughout an organization accessible to decision-makers in an actionable, meaningful and user-friendly format. As the pace of change and degree of risk increases for providers, the need for quick, data-driven decisions grows. Getting data in the hands of operational and clinical leaders will enable improvements in quality, cost and strategy. Whether it's at the bedside or in the executive offices, it is the CIO's duty to get the right information to the right people to provide quality care and make timely, well-informed decisions so the health system runs as effectively and efficiently as possible.
The CIO must be aligned with the strategic priorities of the C-suite. According the annual American College of Healthcare Executives survey, for the 11th year in a row, "financial improvement challenges" topped the list of CEO concerns for 2014, the most recent year available. Not surprisingly, it also tops the list for CFOs, according to several recent surveys.
While CIOs haven't traditionally been financially focused, they are now key players in the cost improvement conversation. The CIO has two vital responsibilities specific to driving out costs: stewardship of the organization-wide IT spend and enabling cost savings initiatives to produce real savings. If a CIO is not viewing his or her role in this way, the organization is undoubtedly not realizing all of the savings available to them.
Stewardship of the IT spend
As healthcare providers become increasingly technology enabled, the opportunities to spend more money on systems, implementation, maintenance fees, networks and consultants are endless. However, the IT stack can quickly become fraught with duplicative systems and functionality — read "excess cost."
After years of cost reduction in front-line operational and clinical areas, it is necessary to look beyond these areas to generate the level of cost savings needed. The CIO should lead the charge to reduce the cost of IT operations.
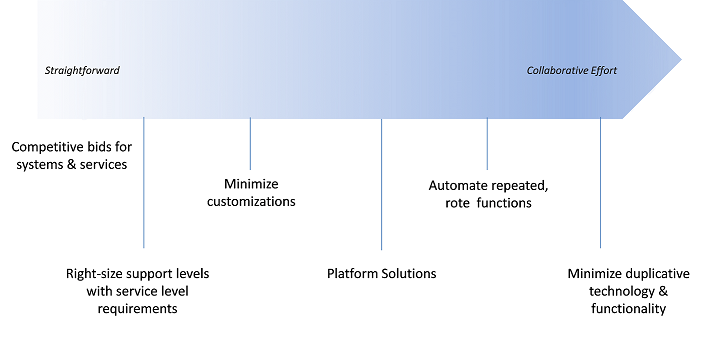
As shown in Exhibit 1, CIO-related cost savings opportunities run the continuum from straightforward just-do-it actions to the more complex initiatives that require cross-functional collaboration and well-defined processes and structures.
Exhibit 1
The power of the platform in reducing cost
One cost savings opportunity that falls directly within the CIO's domain and cannot be overlooked is the power of the platform. Oftentimes, operational, financial or clinical leaders find a system they want that meets their particular needs. But to either feed this system data or use the output of this system, many manual processes are spawned. Smart people become the duct tape that tenuously holds the systems together.
Take the finance operations of a large, academic health system. They have one system for financial decision support, one system for clinical decision support, another system for budgeting, another for long-term financial planning, and yet a fourth system for capital planning and tracking. There are countless manual, offline processes in which a person is critical to moving data from one system to the next. Essential operational reports are routinely run in Excel because no single system supplies the information operational leaders need to manage their department.
Unfortunately, the complexity in this health system is not unique. In fact, it's quite the norm.
It is the CIO's responsibility to provide end users with a better, more efficient, less error-prone process. In the example above, efficiency can be drastically increased by replacing disparate systems with a single platform that provides that functionality all in one.
Reducing customizations
How many times have you heard people in your organization say "we have to customize it to make it work for us" when implementing new systems?
Customizations typically result in higher implementation fees, longer implementation cycles, slower processing times, more support needs, more unplanned downtime and difficulty in upgrading functionality. While it can be difficult to accept off-the-shelf functionality, balancing customizations with standard or supported configurations can result in long-term cost avoidance. It is the CIO's role to help operational and clinical leaders understand this truth and weigh the costs and benefits of requested customizations. Doing so will promote long-term satisfaction with the system.
Simplifying the IT stack to get greater functionality
Having a well-defined methodology for reviewing the existing IT stack and proposals for new systems is an essential CIO duty. The process should include clinical, operational and financial leaders.
Following the DIME method (Exhibit 2) is one example of a rigorous methodology that helps an organization simplify and streamline both existing technologies and evaluate new technologies.
Exhibit 2
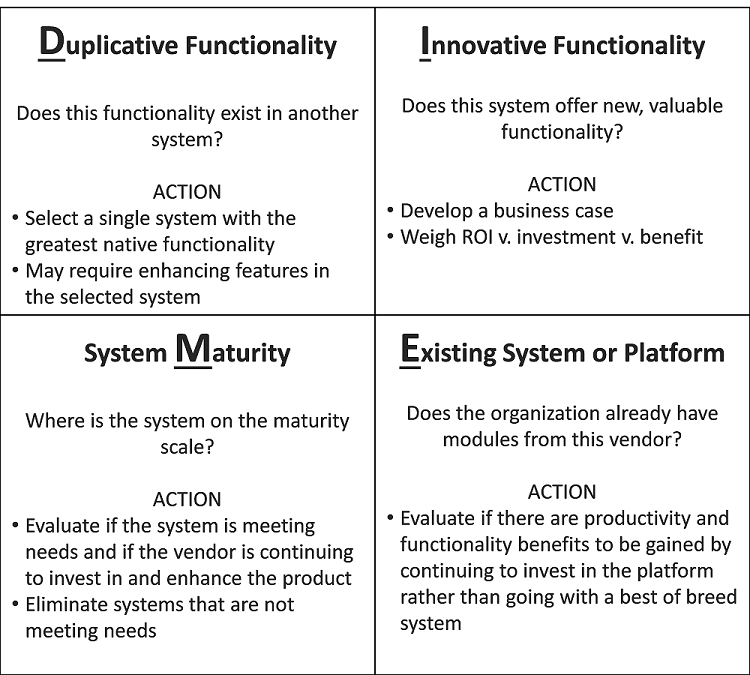
The CIO should require the staff requesting new systems or significant investments in existing systems to provide a business case outlining why the technology is important and the expected ROI on the investment. Clarity and transparency about IT requests, including the expected benefits, allows senior leaders to prioritize how scarce dollars are allocated to produce the highest organizational value. Once systems are implemented, the CIO's office should lead a rigorous look-back analysis comparing the forecasted ROI with the realized ROI.
It is equally important for the CIO to partner with operational, clinical and financial leaders as they work to identify and implement cost savings opportunities.
Promoting self-service access to actionable information
Getting useful, drillable, actionable data into the hands of decision-makers is the most impactful endeavor a CIO can take on. When end users have to go through gatekeepers of information to get data, the pace of change slows dramatically and often comes to a complete standstill. Up until recently, these gatekeepers were instrumental because accessing large amounts of data required deep expertise in writing queries and understanding data structures. However, with the introduction of more user-friendly decision support systems and presentation layer software that sits on top of core systems, many end-users can competently access the data they need to make decisions without gatekeeper assistance.
Providing access to self-service data sources and analytical tools will make an organization more action-oriented, data-driven and focused on metrics that matter.
Overcoming 'integration infatuation'
Integration infatuation occurs when recently affiliated organizations make do with sub-standard or inaccurate information and inefficient processes for their combined entities because they are waiting for the same systems to be adopted throughout. This can take years. In the meantime, manual analyses and unwieldy reports are generated by over-taxed teams. Decision-making and progress on important initiatives stall.
The CIO plays a key role in providing a bridge strategy and technologies that enable business leaders to get the information they need — despite the disparate systems — without waiting for years. Technology can pull the same type of data from different systems, normalize it and then make it available for combined reporting and accessible to decision-makers. Major functional areas, such as billing and financial reporting, can be combined easily and the goal of achieving cost savings through affiliating can be realized sooner.
Recognizing the need for niche technology
Despite huge investments in EHRs, new billing systems and enterprise resource planning systems that promise to fulfill virtually all data and process needs, there are niche technologies that go far beyond the off-the-shelf functionality of large, all-purpose vendors. These niche technologies provide sizeable ROIs. For example, there is technology available that sits on top of the core billing system and automates over 50 percent of the tasks that billing staff do on a daily basis — and with greater consistency.
There is also technology available that runs algorithms to find cost savings across an organization and presents these findings in a way clinical and operational people can easily understand and act on, thus minimizing the need for an army of analysts to do math. It is this type of functionality that can truly change the tenor of an organization. Rather than having people grind through data and invest in automating rote work, staff can focus on work that requires their unique expertise and knowledge. In addition to producing savings by requiring fewer FTEs, these niche technologies can also accelerate the pace of change as staff focuses on driving improvements.
Unfortunately, operational leaders often don't get exposure to these new technologies. The CIO should both scan the market for technologies that will streamline and improve major processes, as well as promote thoughtful consideration of proposals that operational leaders bring forward.
Leveraging the right technology for cost improvement
As CIOs look toward the future and how they can make a positive impact, their No. 1 focus should be expediting the flow of meaningful information into the hands of those who need to make decisions — in all areas of the health system. We know for sure that the technology is there to take healthcare to the next level: to make it more efficient, more predictable, more personalized and more automated. It is the responsibility of the CIO to lead the organization forward in this post-EHR era to a brighter future where healthcare is not only more effective, but also more sustainable for many years to come.
About the Author
Liz Kirk is senior vice president of client services and cost improvement solutions with Strata Decision Technology. With over 15 years of experience working with healthcare providers both as a hospital administrator and a consultant, Liz Kirk is responsible for leading our client services team and the development and delivery of Strata Decision Technology's Continuous Cost Improvement solutions. Liz joined Strata Decision 2 years ago to develop the Continuous Cost Improvement application which is designed to identify and quantify cost savings opportunities, then to drive accountability for realizing true cost savings. Since then, Liz's role has expanded to include leadership of Strata's implementation, optimization, support and project management functions. Prior to joining Strata Decision, Liz was responsible for cost reduction and revenue improvement at Northwestern Memorial Hospital in Chicago, IL. In this role, she led organizational wide initiatives which reduced operating expenses by 17% in two years and added 3% in new net revenue through Charge Capture & Clinical Documentation Improvements.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker's Hospital Review/Becker's Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.

