The shift to value-based care holds much promise, but many healthcare organizations probably feel like they have one foot in two different canoes while trying to navigate the changing market.
A solid footing in the current volume-based model of care is still needed while experimenting with the new models of care that Medicare and other payers are promulgating. The first step into the value-based canoe is to understand the value-based purchasing program, followed by the emerging value-based financial models and the populations that each initiative targets within the healthcare community.
Value-Base Purchasing Programs
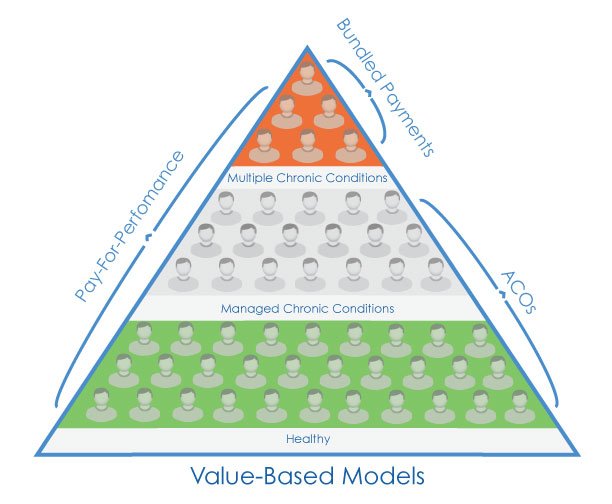
The value-based purchasing models and pay-for-performance programs are designed to improve quality and efficiency within a specific care setting and are similar to other programs which providers have traditionally participated in (i.e., pay-for-performance). One of the major challenges providers face is the new focus on cross-setting (population-based) financial models. New financial models include accountable care organizations which target the healthy and the managed chronically ill populations, as well as bundled payments which target patients with multiple chronic conditions.
Fortunately, there are common themes among these new population programs that can help guide you in the value-based canoe. Here's what you can do today:
1. Pay Attention to Evolving Regulations:
As the new regulations emerge, pay close attention to how they affect your community of care. For example, the following changes allow for better network management by providers in value-based purchasing models:
New ACO regulations allow for incentivizing patients to remain in network and allow patients to be pre-assigned to an ACO.
The recently passed IMPACT Act standardizes quality measurement data across different types of post-acute providers.
2. Take advantage of new codes in volume-base payment systems:
Transitional care codes can help with high-risk, high-cost patients as you move toward bundled payments.
Chronic care management codes can help with ACO initiatives by securing reimbursement for the ongoing care of chronically ill patients.
3. Insure that you are working towards clinically integrated networks (CINS) with your community.
CINs are especially important to care transitions, especially the sharing of metrics and information across the network. Check out my recent blog on Three Things Clinically Integrated Networks Need For Better Care Transitions.
Regardless of the model, the key difference between the new value-based purchasing models and the old fee-for-service models is the need to focus on care across the community, not just within the walls of an organization.
Eric Chetwynd, Director of Product Strategy at Curaspan, ensures that the company continues to deliver solutions that best meet the customers' needs while maintaining the company's position as the market leader in care transitions. He brings more than 15 years of experience creating and leading products to market to his role as the director of product strategy. Prior to joining Curaspan, he helped several healthcare technology companies meet the needs of care management organizations, payer organizations, hospitals, physicians and healthcare consumers. These included Ingenix (OptumInsight), PatientKeeper and IHCIS. Eric holds a BA in Vocal Performance and Music Business from University of Massachusetts Lowell.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker's Hospital Review/Becker's Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.

