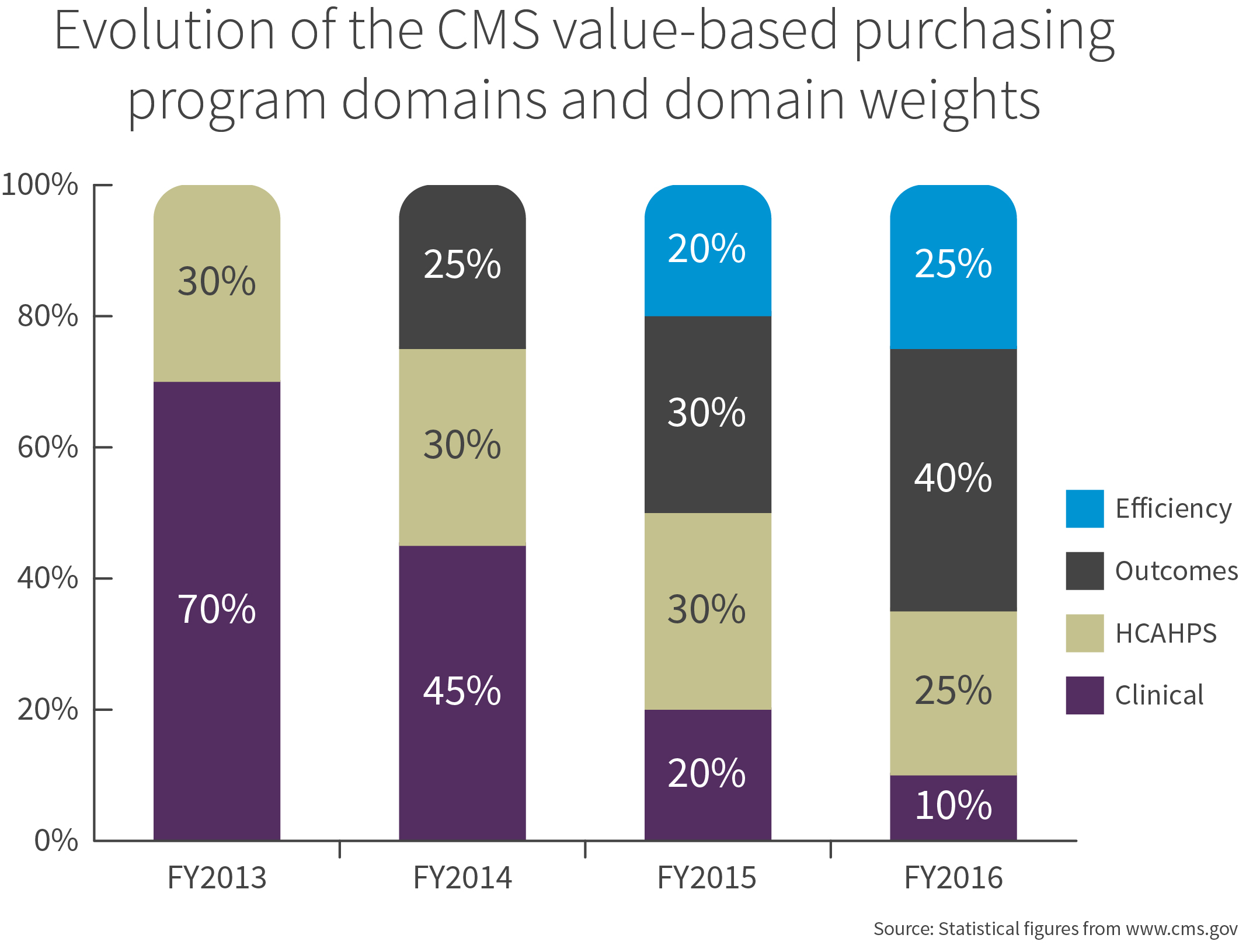
In addition to dealing with pressure to reduce costs, hospital leaders must also manage an evolving array of performance metrics from CMS that determine their reimbursement for care delivered to Medicare and Medicaid patients.
At risk reimbursement will grow over the next several years as the focus moves from clinical process metrics to outcomes and efficiency. Missing performance targets can have significant impacts to a health system's bottom line. Additionally, commercial payers will likely soon adopt similar performance metrics as they shift toward value based payment models.
The good news for hospital leaders is that the work they have done to make service lines efficient, safe and profitable can significantly contribute to their health system's performance for new metrics. Because service lines focus on defined patient populations across the care continuum, they can serve as trailblazers for developing highly efficient processes that promote the coordination between care teams needed for maximum reimbursement in a value based payment environment.
To begin to maximize the potential of your service lines in the new value-based environment here are five areas to focus on now.
1. Leadership model
Service line leadership structures have significantly changed from a hospital clinical leader with an acute care focus to teams of clinicians, physicians and administrators responsible for an episode of care across multiple care settings. Now, 66 percent are now under some type of co-managed structure where dyad and triad teams have some form of joint responsibility for service line performance. A benefit of new service line structures is to create a culture of accountability and empowerment that opens up opportunities for alignment across the care continuum and offers greater fiscal controls, better coordination of care, improved clinical metrics, better patient experience and aligned goals. As you consider alternative service line leadership models that create a foundation for the delivery of value based care and strategic growth, be sure to include:
• As governance structure and organizational alignment with direct or "span of influence" reporting allowing for effective care coordination
• Shared performance goals across the care settings aligned to vision and purpose
• Accurate and timely supply, clinical and operational data for results-oriented decision making across care delivery settings
2. Supply and operational efficiencies
Cost containment is the first half of the value equation. By effectively managing price and utilization as well as waste and variation in supplies and operations hospitals can reduce costs and improve outcomes. To improve supply and operational efficiencies to lower costs, you will need:
• Integrated clinical, operational, supply and financial data analytics that can be used to gauge performance and identify areas of improvement
• Engaged physicians who will champion evidence-based, clinically appropriate utilization and contracting
• Process improvements that reduce variation and standardize supplies
• Optimized workflow in clinical departments to enhance efficiency, productivity, labor resources and revenue
3. Patient care and outcomes
Quality outcomes are the second half of the value equation. Two drivers of high quality outcomes are shared performance goals and adherence to evidence-based utilization guidelines. Start by making sure your clinical staff understands the operational and financial implications of their care delivery. From there, establish physician-developed clinical guidelines, nurse-driven protocols and case management staffing plans that support exceptional patient care and outcomes through:
• Consistent communication between clinical teams and care settings
• Adherence to clinical guidelines and protocols
• Optimal patient flow and care redesign
• Monitoring compliance with established discharge plans
• Zero safety incidents
• Accountability to high patient experience scores
4. Alignment with physician partners
Alignment with physician partners occurs in a variety of ways as organizations shift from volume driven to value driven care and leads to more coordinated and cost effective patient care. Examples of alignment in the beginning stage are medical directorships, service line steering committees and professional service contracts. As the shift progresses, alignment becomes more organizationally integrated with higher levels of shared accountability for cost and outcomes such as joint ventures, service line co-management and pay for performance. More fully aligned organizations are distinguished by physician employment, formal clinical integration and alternative payment models such as accountable care organizations and bundled payments.
Every system needs to evaluate their current physician relationships and develop a formal strategy around how to advance it over time with shared goals and responsibility because informal structures do not provide the alignment needed for value based environment.
5. Strategic growth and profitability
Creating a service line approach focused on strategic growth and profitability across the care continuum is the last critical area of focus. Executive and service line leaders need to start by understanding the current and future state of patient volume and competitive dynamics in their market. This should include evaluating the most cost effective, appropriate site of care, and planning for the necessary infrastructure to support future demand, whether that be through people, facility, technology or clinical program needs.
CMS's change to its reimbursement for Medicare beneficiaries to include an efficiency measure this year is just the leading edge of the wave that is pushing the industry towards a value based system of care. To be successful, leaders will need to think broadly about how to maximize the value of a health system versus an individual hospital including strategic alliances with traditional competitors or community based organizations.
Taking steps now to evolve your service lines through hospital-physician alignment can help organizations create the standardized pathways for the patient-centered, multidisciplinary care that will be critical to succeed in the new healthcare environment. Doing all of this while remaining profitable will require creative skill but can lead to becoming a payer-preferred provider in a value based, competitive environment.
Lani Berman is the Vice President of Performance Services for VHA Inc. Her team of consultants helps members improve supply chain, clinical, operational, financial and strategic performance in high-cost service lines including cardiovascular, orthopedic and spine. She has more than 20 years of experience in healthcare and benefits consulting as well as pharmaceutical marketing.

