Most hospital CEOs realize how payment trends affect the surgery department. New payment models are making it more important than ever for hospital ORs to increase quality, improve outcomes and control costs. Few hospital leaders, however, understand how surgeon income impacts OR performance. The fact is that changes in surgeon economics will soon have a profound effect on OR revenue.
How? Surgeons have always been key to bringing business to the OR. Today they are also critical to helping ORs thrive under new quality-based payment models. Yet most surgeons are struggling financially in the current environment. Malpractice and clinic costs are escalating, and overall reimbursement is static or decreasing. Hospitals that fail to support surgeons will suffer a double hit — declining OR volume as surgeons move cases to competing facilities and declining payment as the OR struggles alone to address quality shortfalls.
What can hospital CEOs do to protect OR revenue? The first step is to understand how the current surgical services environment affects hospital ORs and their surgeon partners.
The new surgical services environment
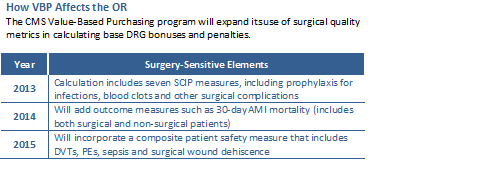
OR revenue is shifting from quantity- or volume-based reimbursement to quality- or outcomes-based payment. Medicare has not paid for care related to preventable problems like surgical site infections and retained objects since 2008. Starting in 2015, CMS will begin exacting a 1 percent DRG penalty on hospitals with high rates of these and other healthcare-acquired conditions. The CMS Hospital Value-Based Purchasing program currently tracks several surgical process metrics, and it will incorporate more surgical quality measures in the coming years (see "How VBP Affects the OR" below). In addition, Medicare readmission penalties may expand to cardiovascular surgery in 2015.
New Medicare programs are also pushing ORs to foster greater cost control. Under the Medicare ACO and bundled payment initiatives, high surgery department costs may erode any shared hospital savings. Private insurers are also introducing quality-based payment and shared savings methodologies. Taken together, these payment trends are squeezing revenue for many hospital ORs.
Meanwhile, the margins are also narrowing for surgeons. Surgical specialists have been experiencing declining reimbursement for years. Now, the Patient Protection and Affordable Care Act proposes a 24 percent decrease in reimbursement for surgeons who fail to meet certain quality metrics. At the same time, practice costs are escalating, with malpractice costs and health insurance premiums leading the way. Together, payment reductions and cost increases are suppressing surgeon incomes. Some surgeons are working longer hours to maintain revenue, but many are curtailing their practice or quitting medicine altogether.
All of these trends are combining to put hospitals in a vice. Declining payment is suppressing revenue on one side, and surgeon struggles are leading to declining case volumes on the other. The good news is that four core strategies can address both problems simultaneously.
1. Involve surgeons in OR leadership
Surgeon demands for schedule access, rich staffing and new technology have helped create costly ORs. Yet surgeon-owned ambulatory surgery centers prove that surgeons can run lean, cost-efficient surgery organizations. How can hospitals harness that management skill? Many hospitals have established effective surgeon leadership by creating a Surgical Services Executive Committee.
Think of an SSEC as an operational "board of directors" for the OR. An effective SSEC is led by surgeons and includes representatives from anesthesia, nursing and hospital administration. Its mission is to manage OR access, improve OR operations and optimize clinical safety and outcomes.
Hospital CEOs often fear the idea of a surgeon committee running the OR. Will it become just a forum for new demands and increased headaches? These fears are unfounded. Surgeons welcome the opportunity to take greater responsibility for the OR, and well-designed SSECs conscientiously work to optimize department efficiency, resource use, clinical quality and overall financial performance.
2. Create an efficient work environment for surgeons
Surgeons want to be able to access the OR schedule when needed, start their day on time, provide high-quality care and be as productive as possible. At the same time, hospitals need to make the most efficient use of the OR.
In most hospitals, the top priority is to restructure the block schedule system. Block system reform can be complex, but two principles are key:
- Shorter blocks (4 to 6 hours) are less efficient than longer blocks (8+ hours). Longer blocks maximize efficiency in a vertical manner by creating consistency in the labor and non-labor resources required to improve overall productivity.
- Utilization thresholds are imperative. Most ORs do not require surgeons to use assigned block time efficiently. Well-run ORs set a utilization threshold of 75 to 85 percent as the requirement for maintaining ownership of a block.
Other block system changes help ensure schedule flexibility. In addition, ORs need to examine nursing processes to ensure strong clinical support and efficient turnover. Data-driven decision making is critical to productivity — key stakeholders should have access to clear and transparent performance dashboards and operational metrics. Taken together, these schedule and process improvements allow surgeons to maximize their case volume, sustain their income and improve their lifestyle through greater predictability. They also ensure the optimal use of the hospital's expensive OR resources.
3. Build quality into the system
New payment models are putting ORs on the hook for surgical complications and poor patient outcomes. One core solution is to build quality into the system through standardized preoperative processes.
Single-path scheduling. In many ORs, the case scheduling process is disorganized and inefficient. OR staff and surgeons fail to capture complete information on patients for scheduled procedures. Better-performing ORs create a "single pathway" for the scheduling process to ensure quality, remove variability and prevent errors. Develop a standardized fax form (or IT/IS module) with required fields for patient identifier, specific procedure information, patient co-morbidities and other critical details. Standardized scheduling processes ensure that OR staff are able to identify and manage all patient risk factors ahead of surgery.
Pre-surgical testing. In most ORs, pre-surgical evaluation is incomplete, expensive or both. In better-performing hospitals, the SSEC creates pre-surgical testing and patient management protocols specific to disease, procedure, co-morbidities and other risk factors. Integrating case management, anesthesia and hospitalists into pre-surgical processes is important to improving clinical outcomes. Well-designed testing and preparation protocols help ensure patients are optimized for their procedure and for a speedy recovery.
Daily huddle. In better-performing ORs, a multi-disciplinary caregiver group takes 20 to 30 minutes every afternoon to review the next day's schedule. The purpose of this "daily huddle" is to verify patient preparation, reschedule patients who are not ready for surgery and flag any potential problems with the schedule, equipment, etc. An effective huddle not only increases patient safety, it reduces case delays and cancellations and ensures the schedule runs as smoothly as possible.
4. Create the systems and culture of safety
For the typical hospital, Medicare HAC penalties could amount to $250,000 or more per year. The key to avoiding errors and preventable complications is to embed safety in OR processes. Tackle the issue from several angles:
Checklists. Implementing the World Health Organization's Surgical Safety Checklist as part of the universal safety protocols ensures that staff use safe processes 100 percent of the time. In many ORs, safety checklists have been instrumental in reducing sentinel events and improving quality metrics.
Crew resource management. Adapted from the aviation industry, CRM is a set of principles that support clear communication about risks. CRM flattens hierarchies and empowers all staff to take responsibility for patient safety.
Hospital surgery departments also need to foster a "just culture" focused on learning from mistakes, not assigning blame. Modeled by leadership, a just culture allows staff to be honest about quality lapses without finger pointing and put energy into fixing broken processes. In addition, anonymous error reporting helps ensure that safety events are brought to light so that staff can identify root causes and prevent future recurrences.
Case Study: CarolinaEast
Implementing the four strategies described above can have a significant impact on both a hospital OR and its surgeon partners. CarolinaEast Health System runs a 12-room hospital OR (10 rooms currently operational) and a six-room outpatient surgery center in New Bern, N.C. In 2009, the surgical services department was facing declining case volume and high surgeon dissatisfaction.
In 2010, CarolinaEast took a series of steps to turn around OR performance. Interventions included creating a physician-led SSEC to run the OR, strengthening the block schedule system, creating a protocol-driven Pre-Admission Testing Center and implementing a daily huddle. The OR also implemented several safety initiatives.
In less than a year, OR utilization at CarolinaEast increased from 48 to 73 percent. After one year, average monthly case volume had increased approximately 8 percent. Better patient management and safety processes led to improved quality metrics. Patients were better prepared for surgery and length of stay decreased. From the surgeon perspective, schedule access and practice efficiency improved markedly. Surgeon complaints declined, and surgeons started steering more cases to the OR.
Financial synergy
Hospitals like CarolinaEast are well positioned to thrive in the evolving surgery market. Strong surgical quality metrics help maintain revenue under quality-driven payment models. In addition, higher utilization creates a leaner cost structure, enabling ORs to do well under shared savings arrangements.
Surgeons benefit as well. Many well run ORs have leveraged quality gains to negotiate payer contractual bonuses for surgeons, and efficiency improvements allow surgeons to optimize their productivity. These gains reinforce surgeon satisfaction, engagement and loyalty, driving strong OR revenue and volume.
William Panza, MD, is a board-certified anesthesiologist who practices in New Bern, NC. Dr. Panza is also a consultant with Surgical Directions, a physician-led consulting firm that helps hospital ORs improve clinical outcomes, financial performance, and patient and staff satisfaction. Robert Dahl is senior vice president and chief operating officer at Surgical Directions. They can be reached at (312) 870-5600.
More Articles on OR Operations:
5 Reasons Hospital ORs Score Low on Key Quality Measures
3 Ways to Save Costs in the OR
6 Cornerstones of Operating Room Efficiency: Best Practices for Each

